Mallet Finger – Diagnosis and Treatment
Orthopedic, Trauma
Context
- The term mallet finger refers to injury of the extensor tendon of the distal interphalangeal (DIP) joint, resulting in loss of active extension of the DIP joint and a DIP joint that rests at roughly 45° flexion (1,2).
- The injury can range from partial tear to complete rupture of the extensor tendon, which can cause avulsion of the distal phalanx (mallet finger fracture) (1).
- The mechanism of injury commonly involves a traumatic forced flexion of the distal phalanx when in the extended position (3). A mallet finger can also result from a sharp or crushing laceration to the dorsal DIP joint.
- This injury is commonly encountered in sports following forceful flexion of the distal phalanx.
Diagnostic Process
- Diagnosis of mallet finger injuries can be made with physical examination, history, and radiographs (3).
- Patients will typically present with pain in the affected joint, deformity, and an extensor deficit at the DIP joint. There is often a forced flexion or hyperextension injury of the DIP joint (3).
Mallet injuries can be classified according to the Doyle System (4):
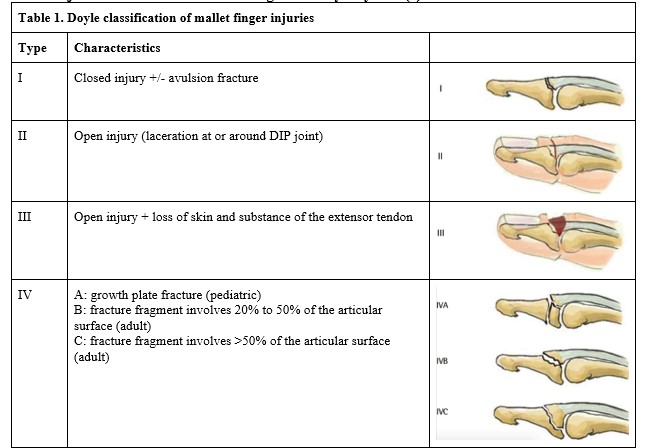
Images accessed from Open-i (https://openi.nlm.nih.gov/detailedresult?img=PMC4807168_aps-43-134-g005&query=&req=4&it=xg) CC BY NC 4.0
Recommended Treatment
The goal of treatment is to restore DIP joint extension and prevent a swan neck deformity (1, 3).
Non-surgical treatment:
- Most mallet finger injuries can be treated non-surgically. Commonly reported indications for non-surgical treatment include closed injury and a fracture fragment size that is < ⅓ of the joint surface area (1,3).
- Non-surgical treatment involves applying a splint on the volar or dorsal aspect of the finger to maintain the DIP joint in extension for 6-8 weeks (1,3). There are many different types of splints that can be used – aluminum foam, plastic, or custom-made thermoplastic – and none have been proven to be superior to another (3,5).
- Complications that can occur from splinting include allergic reaction to tape, skin ulceration, and splint-related pain (6).
- The main challenge with splinting is patient compliance.
Surgical treatment:
- Indications include size of fracture (more than one-third of articular surface involvement) and subluxation of the distal phalanx (1,3).
- Surgical techniques include trans-DIP joint K-wire fixation, open reduction internal fixation with K-wire, and open suture repair of the tendon plus trans-DIP joint K-wire fixation (1).
- Complications that can occur include nail deformity, infection, and hardware failures (1,3).

Figure 1. Splinting of dorsal DIP joint. Image accessed from Open-i (https://openi.nlm.nih.gov/gridquery?q=mallet%20finger&m=1&n=100&it=xg) CC BY NC 4.0
Criteria for Consult
- Referral to plastic surgery for outpatient follow-up.
Criteria For Safe Discharge Home
- Patient can be discharged home with splint and follow-up instructions.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
High quality. There is a wide range of studies and systematic reviews with small variation between studies.
Related Information
Reference List
Lin JS & Samora JB. Surgical and Nonsurgical Management of Mallet Finger: A Systematic Review. J Hand Surg Am. 2018 Feb;43(2):146-163.e2. Epub 2017 Nov 22. https://doi.org/10.1016/j.jhsa.2017.10.004
Lamaris GA & Matthew MK. The Diagnosis and Management of Mallet Finger Injuries. Hand (N Y). 2017 May;12(3):223-228. Epub 2016 Mar 30. DOI: 10.1177/1558944716642763.
Bloom JMP, Khouri JS, Hammert WC. Current concepts in the evaluation and treatment of mallet finger injury. Plast Reconstr Surg. 2013;132(4):560e-566e.
Doyle JR. Extensor tendons: acute injuries. In: Green DP, Pederson CW, Hotchkiss RN, eds. Green’s Operative Hand Surgery. 4th ed. New York, NY: Churchill Livingstone; 1999:195-198.
Cheung JPY, Fung B, Ip WY. Review on mallet finger treatment. Hand Surg. 2012;17(3):439-447.
Katzman BM, Klein DM, Mesa J, Geller J, Caligiuri DA. Immobilization of the mallet finger: effects on the extensor tendon. J Hand Surg. 1990;24:80-84.
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 29, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.