Mesenteric Ischemia
Gastrointestinal
Context
- Mesenteric ischemia is uncommon cause of abdominal pain:
- Less than 1 in 1000 hospital admissions.
- However, mortality rate is high if diagnosis is delayed or missed.
- Clinical starting point:
- Have high index of suspicion and low threshold to CT, especially in patient presenting with acute abdominal pain and cardiovascular risk factors.
- Clinical endpoint:
- Disposition depends on etiology of ischemia, with better prognosis for venous rather than arterial etiology, and chronic rather than acute ischemia.
- Patients with acute arterial ischemia are often very ill and prognosis guarded.
- Chronic mesenteric ischemia is often caused by atherosclerosis and can be debilitating due to postprandial pain, food fear, and weight loss.
- However, not acutely fatal and will not be considered further in this clinical summary.
- Etiology:
- Mesenteric arterial occlusion:
- Embolic source: 40-50%
- Thrombotic occlusion: 20-35%
- Dissection: <5%
- Mesenteric venous thrombosis: 5-15% of cases
- Primary (idiopathic)
- Secondary causes: thrombophilia, trauma, local inflammatory changes from pancreatitis, diverticulitis, inflammation, or infection, etc.
- Nonocclusive mesenteric ischemia: 5-15% of cases
- Cardiac insufficiency or low-flow states.
- Increasingly identified in patients undergoing hemodialysis.
- Mesenteric arterial occlusion:
Diagnostic Process
- Risk factors:
- Mesenteric arterial occlusion:
- Arterial embolism: atrial fibrillation and other atrial tachyarrhythmias, recent MI or other embolic events (e.g.: stroke), less commonly cardiac valvular disease, endocarditis, proximal aneurysm, recent catheter-based angiography.
- Arterial thrombosis: atherosclerosis.
- Mesenteric venous thrombosis:
- DVT
- Hx of cancer, chronic liver disease.
- Recent abdominal surgery.
- Thrombophilia or family history of clotting disorders.
- Nonocclusive mesenteric ischemia:
- Low-flow states: severe heart failure, severe sepsis.
- Recent cardiac surgery.
- Hemodialysis.
- Mesenteric arterial occlusion:
- History:
- Look for evidence of atherosclerotic and vascular disease on history:
- PAD, CVS, CAD
- History of atrial fibrillation and recent MI hints to possible embolic source.
- History of low-flow states such as severe cardiomyopathy points to non-occlusive source.
- Wide spectrum of nonspecific patient presentations makes the diagnosis challenging:
- Can vary from pain out of proportion to vague abdominal pain to absent abdominal symptoms altogether.
- Classic triad: look for sudden, severe abdominal pain, gut emptying with vomiting/diarrhea, underlying cardiac disease.
- Embolic source more likely if acute onset of ischemic symptoms in previously asymptomatic patient, with no prodrome and rapid progression.
- Thrombotic source more likely if sudden worsening of symptoms in a patient with long history of intestinal angina.
- Look for evidence of atherosclerotic and vascular disease on history:
- Physical exam:
- Nonspecific
- Classically, pain out of proportion to exam should prompt the physician to consider mesenteric ischemia.
- Absent bowel sounds, fecal occult blood are late findings.
- Tachycardia, tachypnea, hyper or hypothermia.
- Hypotension is late and ominous finding.
- Investigations:
- CT angiography is the gold standard,
- CBC: elevated WBC may indicate full-thickness injury to bowel wall or ischemia with bacterial translocation,
- Electrolytes
- Metabolic acidosis
- Lactate: often elevated late in disease; significant elevation associated with patient mortality,
- ECG: look for arrhythmias such as atrial fibrillation.
- Imaging: abdominal x-ray, duplex ultrasound, CT angiography.
- X-ray may show bowel distention with air-fluid levels, progression to necrosis manifests as pneumatosis intestinalis (linear collections of air in bowel wall).
- Duplex ultrasound has high sensitivity and specificity but can be difficult to obtain due to degree of pressure applied. It is best reserved for chronic mesenteric ischemia.
- CT angiography has 95-100% accuracy and has become recommended method of imaging for diagnosis of visceral ischemic syndromes.
- Decreased or absent bowel wall enhancement is most specific CT sign of intestinal ischemia.
- Non-specific findings taken together are more specific for acute mesenteric ischemia: bowel wall thickening, mesenteric edema, luminal dilatation of intestine, portal venous gas.
Management
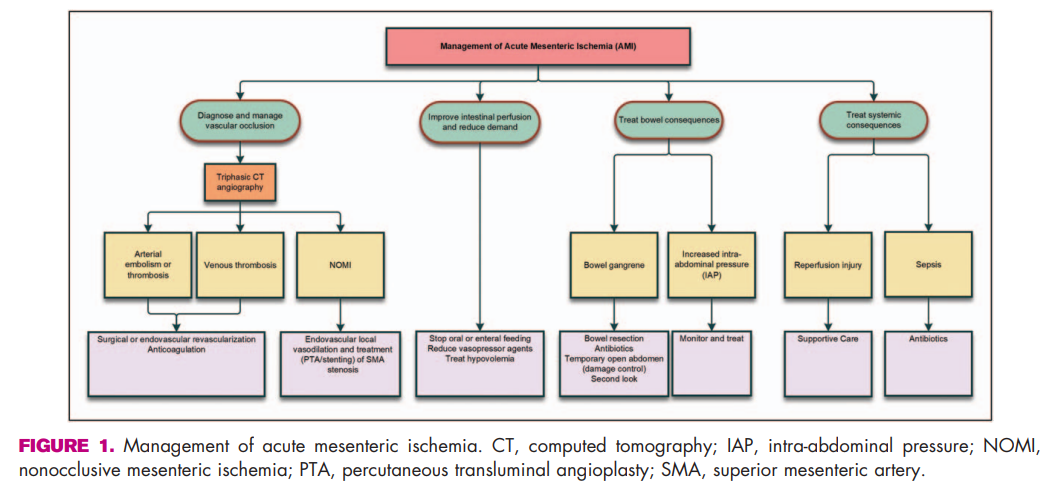
Figure taken from article by Blaser et al. A clinical approach to acute mesenteric ischemia. Current Op in Crit Care. 2021; 27: 183-92
Mesenteric Arterial Ischemia:
- Initial management:
- Aggressive IV fluids and electrolyte monitoring, AVOID vasopressors.
- IV broad-spectrum antibiotics.
- IV unfractionated heparin: decision should be made with surgical consult.
- NPO in acute mesenteric ischemia.
- Enteral nutrition or parenteral nutrition in chronic mesenteric ischemia.
- Stable: endovascular intervention with pharmacomechanical thrombolysis (embolic disease) or stenting (thrombotic disease).
- Unstable: laparotomy with thromboembolectomy, mesenteric bypass and/or retrograde mesenteric stent, and bowel resection, if necessary.
Mesenteric Venous Thrombosis:
- Stepwise approach:
- If symptoms are mild and no CT evidence of compromised bowel perfusion, LMWH and transition to oral anticoagulation.
- If symptoms are severe and CT shows edematous bowel, continuous IV UFH.
- If medical treatment fails, options include percutaneous mechanical thrombectomy and/or catheter-directed thrombolysis via transhepatic access.
- Any evidence of peritonitis, stricture, GI bleed should prompt exploratory laparotomy.
Nonocclusive Mesenteric Ischemia:
- Ensure hemodynamic stability: fluid resuscitation and electrolytes, blood transfusion.
- Manage underlying cause (HF or sepsis).
- IV infusion of vasodilatory and antispasmodic agents can be used:
- Papaverine 60 mg bolus followed by infusion (30-60 mg/hr) with repeated angiograms obtained every 24 hours.
- Laparotomy when bowel necrosis is suspected.
Long-term management:
- Aspirin lifelong in all patients who undergo endovascular or open repair.
- Clopidogrel for 1-3 months after endovascular repair.
- DOAC indicated in patients with atrial fibrillation, MVT.
- Lifestyle management: smoking cessation, exercise, manage dyslipidemia and hypertension.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Society guidelines and critical reviews.
Related Information
OTHER RELEVANT INFORMATION
EM Board Bombs: https://www.emboardbombs.com/papers/2020/3/9/the-abominable-pain-acute-mesenteric-ischemia
Emergency Medicine Cases Podcast: https://emergencymedicinecases.com/episode-42-mesenteric-ischemia-pancreatitis-3/
Life in the Fast Lane: https://litfl.com/mesenteric-ischaemia/
Reference List
Bala M, Kashuk J, et al. Acute mesenteric ischemia: guidelines of the World Society of Emergency Surgery. Wor J of Emerg Surg. 2017; 12: 38-49.
Blaser AR, Acosta S, Arabi YM. A clinical approach to acute mesenteric ischemia. Current Op in Crit Care. 2021; 27: 183-92.
Clair DG, Beach JM. Mesenteric Ischemia. New Eng J Med. 2016; 374: 959-68.
Hawkins BM et al. Endovascular Treatment of Mesenteric Ischemia. Cathet and Cardio Interv. 2011; 78: 948-52.
Karkkainen JM, Acosta S. Acute mesenteric ischemia (part I): Incidence, etiologies, and how to improve early diagnosis. Best Prac & Res Clin Gastro. 2017; 31: 15-25.
Karkkainen JM, Acosta S. Acute mesenteric ischemia (part II): Vascular and endovascular approaches. Best Prac & Res Clin Gastro. 2017; 31: 27-38.
Martinez JP, Hogan GJ. Mesenteric ischemia. Emerg Med Clin of North Am. 2004; 22: 909-28.
Zhao Y, Yin H, et al. Management of Acute Mesenteric Ischemia: A Critical Review and Treatment Algorithm. Vasc and Endovasc Surg. 2016; 50(3): 183-92.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 19, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.