Myositis Ossificans
Other
Context
- Myositis ossificans (MO) is a benign ossifying lesion that can affect any type of soft tissue, including subcutaneous fat, tendons, and nerves. It is most commonly found in muscle as a solitary lesion within athletes.
- The pathophysiology is not fully understood, but in most cases, lesions develop around areas of previous injury or repetitive trauma. Patients present with pain and/or decreased range of motion in cases of periarticular lesions. In severe cases, lesions may have compressive effects on nervous structures.
- Importantly the role of the emergency physician is to begin the diagnostic work-up to differentiate MO from more sinister lesions (eg. sarcoma) if radiographically ambiguous. In early cases of MO when calcification is incomplete, radiographs will be non-diagnostic. These cases may require follow-up investigation including CT, MRI, biopsy, or as guided by orthopedic surgeons.
- In well-calcified lesions with a history of trauma, MO is a self-limited self-resolving issue in most patients. Treatment is similar to acute soft-tissue injuries, with an initial rest and ice/compression/analgesia phase, followed by increasing range of motion as tolerated. In sustained cases, physiotherapy is necessary to help improve function and refractory cases may be considered for operative excision by an orthopedic surgeon.
Diagnostic Process
- The diagnosis of MO is made through a combination of history, physical exam, and plain radiography in the majority of cases. The location can be anywhere but due to injury patterns occurs most frequently in the arm flexors and thigh extensors.
- A history of trauma or repetitive injury is classic though not required, and patients present with pain or decreased range of motion due to mechanical irritation. Examinations reveal non-specific muscle belly or peri-articular tenderness with decreased ROM if peri-articular.
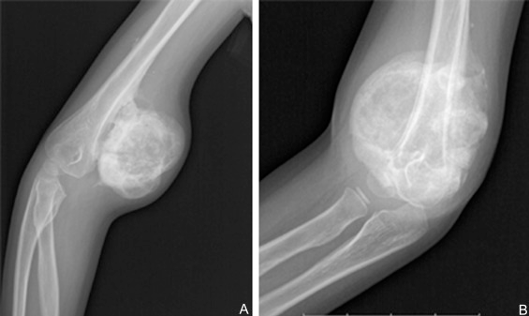
- Radiologic investigations are primary method for diagnosis, with histological assessment being the gold standard. Plain radiographs or CT scans that are performed will demonstrate well-calcified lesions separate to bone in those that are mature (4-6 months). Discussion with radiology regarding the nature of the heterotopic calcified lesions can confirm the diagnosis.
Li PF, Lin ZL, Pang ZH. Non-traumatic myositis ossificans circumscripta at elbow joint in a 9-year old child. Chin J Traumatol. 2016 Apr 1;19(2):122-4.
- The important pitfalls related to diagnosing MO occur predominantly in acute and subacute lesions adjacent to bony tissue. These will demonstrate poorly localized periosteal soft tissue swelling with irregular calcification. Cases that are not clearly well-calcified heterotopic foci separated from bone all require orthopedic referral and follow up imaging with MRI. The differential diagnosis includes periosteal osteosarcoma, synovial sarcoma, and malignant fibrous histiocytoma which cannot be excluded on initial radiograph in early cases of MO.
Recommended Treatment
- Treatment for definitive cases diagnosed in the emergency room are symptom-guided and targeted towards function:
- Tylenol and NSAIDs if appropriate for analgesia
- Initial rest if an acute injury is superimposed on a chronic calcified lesion
- Physiotherapy for improving range of motion
- Refractory cases or repeat presentations merit orthopedic referral for consideration of lesion excision.
- These patients do not require admission, transfer, or inpatient consultation.
- Diagnostically uncertain cases require orthopedic referral for consideration of advanced imaging and further diagnostic work-up.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The radiological specificity to make this diagnosis has been well-studied and described for mature lesions; unfortunately, the heterogeneity and rarity associated with early presentations has prevented reliable diagnostic criteria for emergency-based presentations. The evidence is mainly case-series in quality which has significant selection bias towards atypical cases; however, within the ED, binary decisions can still be made from this pool of literature whereby cases are either highly specific pathognomonic lesions or atypical requiring follow-up.
Related Information
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 22, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…



POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.