Myxedema Coma
Critical Care / Resuscitation, Metabolic / Endocrine
First 5 Minutes
- Myxedema coma is a critical, life-threatening decompensation of hypothyroidism requiring rapid recognition and treatment.
- These patients should be placed in a resuscitation bay on a monitor with advanced airway equipment at the bedside.
- Treatment must often be started empirically with potentially toxic doses of thyroid hormone that may precipitate thyroid storm.
Context
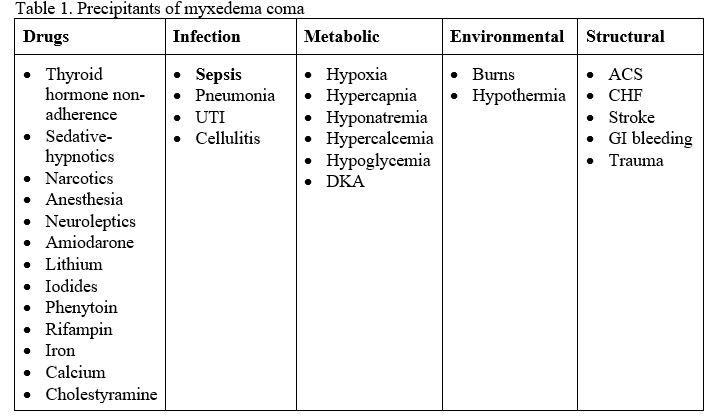
- Myxedema coma or decompensated hypothyroidism is characterized by the triad of altered mental status, hypothermia and a precipitating event. The triggers of myxedema coma can be remembered with the DIMES mnemonic (see Table 1).
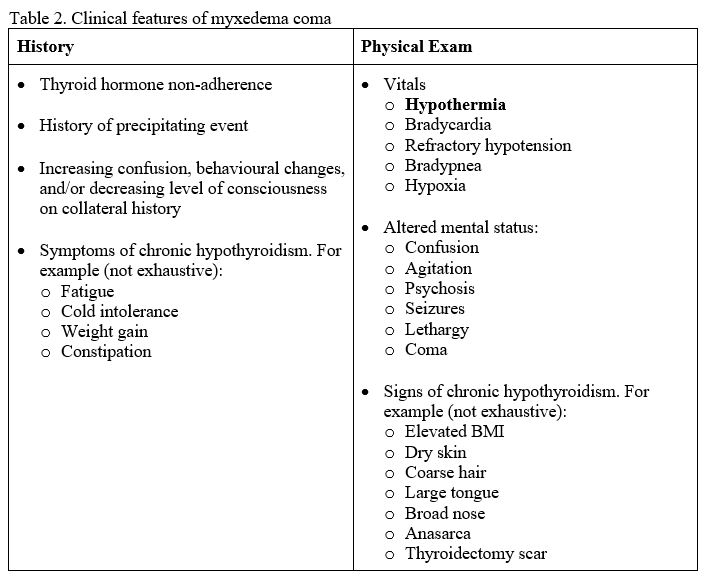
- The typical patient profile is an older female with signs of severe chronic hypothyroidism presenting in the winter. The clinical features of myxedema coma are listed in Table 2.
- The differential diagnosis of myxedema coma is broad and can be approached with the DIMES or AEIOU TIPS mnemonics for altered mental status.
Diagnostic Process
- Myxedema coma is often a clinical diagnosis with support by a severely elevated TSH.
- Two clinical decision tools have been developed. Rosen’s recommends the Myxedema Coma Screening Tool to aid in diagnosis and treatment decisions (specificity and sensitivity of ~80%). However, this tool requires further validation and should be used with caution. Early consultation with internal medicine, endocrinology, and/or critical care is indicated to assist in diagnosis and management.
Criteria:
- GCS
- 0-10: 4 points
- 11-13: 3 points
- 14: 2 points
- 15: 0 points
- TSH
- >30 mU/L: 2 points
- 15-30 mU/L: 1 point
- Free T4
- <7.72 pmol/L: 1 point
- Hypothermia
- <35°C: 1 point
- Bradycardia
- <60 bpm: 1 point
- Precipitating event
- See Table 1: 1 point
Total Score and recommendations:
- 8-10: diagnosis is most likely; treat
- 5-7: likely; treat if no alternative diagnosis
- <5: unlikely; consider alternative diagnosis
Recommended Treatment
- Supportive care and stabilization
- Large bore IV access.
- Monitors.
- Intubation and ventilation, if indicated.
- Hypotension
- Gentle fluid resuscitation with NS +/- dextrose to treat any concomitant hyponatremia and hypoglycemia (use fluids with caution as aggressive volume resuscitation can unmask CHF).
- Early IV thyroid hormone (see below).
- Some patients may require vasopressor support (e.g., norepinephrine) until thyroid hormone replacement takes effect.
- Hypothermia
- Passive rewarming with blankets to prevent further heat loss.
- If active rewarming, pre-treat and monitor for hypotension.
- Hyponatremia and/or hypoglycemia
- Treat as above and per standard protocol.
- IV thyroid hormone replacement
- Levothyroxine (T4)
- Loading dose
- 4 mcg/kg IV (~200-400 mcg).
- 100 mcg if elderly, small or history of coronary artery disease or arrhythmia.
- Maintenance
- 100 mcg IV 24 hours later, then 50 mcg IV q daily until tolerating PO (1.6 mcg/kg PO daily).
- Loading dose
- Add triiodothyronine if persistent hemodynamic instability or poor respiratory effort. However, use with caution in cardiac patients due to risk of arrhythmias or infarction.
- Loading dose
- 5-20 mcg IV
- 5-10 mcg if elderly, small or history of coronary artery disease or arrhythmia
- Maintenance
- 2.5-10 mcg IV q8H until patient is conscious and tolerating PO
- Loading dose
- Levothyroxine (T4)
- Stress dose steroids for possible adrenal insufficiency.
- Hydrocortisone 100-200 mg IV q8H.
- Identify and treat precipitating factors (see Table 1).
Criteria For Hospital Admission
Patients with myxedema coma require admission, endocrinology evaluation, and, depending on severity, ICU consultation.
Criteria For Transfer To Another Facility
- Depends on local guidelines.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Most of this resource is based on high-quality evidence from emergency medicine texts. The Myxedema Coma Screening Tool is based on low-quality evidence: it was derived from a single-centre, retrospective chart review with a small sample size and requires further validation.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Thiessen MEW. Thyroid and Adrenal Disorders. In: Walls RM, Hockberger RS, Gausche-Hill M, Erickson TB, Wilcox SR, editors. Rosen’s Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia (US): Elsevier; 2023. p. 1566-1585.
Cimino-Fiallos N. Decompensated Hypothyroidism. In: Mattu A, Swadron S, editors. CorePendium [Internet]. Burbank, CA: CorePendium, LLC; 2021 Jan 07 [cited 2023 May 24]. Available from: https://www.emrap.org/corependium/chapter/recq2Rb31DrFS9QWD/Decompensated-Hypothyroidism#h.qgt33a39yakc
Chiong YV, Bammerlin E, Mariash CN. Development of an objective tool for the diagnosis of myxedema coma. Transl Res [Internet]. 2015 Jan [cited 2023 May 24];166(3):233-43. Available from: http://dx.doi.org/10.1016/j.trsl.2015.01.003
Idrose A. Hypothyroidism and Myxedema Crisis. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH, editors. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide [Internet]. 9th ed. United States: McGraw Hill Medical; 2020 [cited 2023 June 7]. Chapter 228. Available from: https://accessmedicine.mhmedical.com/content.aspx?sectionid=190237546&bookid=2353&Resultclick=2
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 15, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.