Nail Bed Injury and Repair
Orthopedic, Trauma
First 5 Minutes
- X-rays generally needed.
- 50% of nail bed injuries are associated with fracture. Most are comminuted tuft fractures which don’t require specific treatment beyond splinting.
- Ensure tetanus UTD.
Context
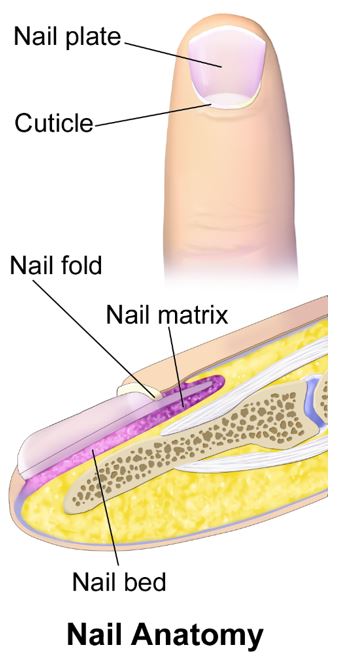
- Nail bed injuries include subungual hematoma (see resource https://emergencycarebc.ca/clinical_resource/subungual-hematoma-treatment/), nail bed avulsion, and laceration of the nail bed.
- Related injuries include DIP dislocations or fractures.
Search media – Wikimedia Commons [Internet]. commons.wikimedia.org. [cited 2024 Jan 12]. Available from: https://commons.wikimedia.org/w/index.php?search=nail+anatomy&title=Special:MediaSearch&go=Go&type=image
- Nail bed wounds generally heal within two weeks; a nail will generally regrow in 3 months.
Diagnostic Process
- Assess for intact range of motion/tendon injury, and neurovascular status.
- First step in diagnosis is assessing for subungual hematoma, presence of laceration and/or avulsion.
- Assess whether the nail plate is intact.
- Finger x-ray for distal phalangeal fracture which may alter treatment.
Recommended Treatment
- Subungual hematoma: If present and less than 50% of the nail bed, see the subungual hematoma treatment clinical resource. (https://emergencycarebc.ca/clinical_resource/subungual-hematoma-treatment/)
- Tetanus updated as needed.
- Prophylactic antibiotics: for excessive contamination or immunocompromised status.
- General preparation: perform a digital block with two mL of lidocaine into the proximal digital crease. If available apply a finger tourniquet for a maximum of two hours. Irrigate with copious sterile saline or tap water (which have been shown to have no different in infectious outcomes).
- Nail removal: If indicated (ex. subungual hematoma greater than 50% of nail bed, concern for open fracture, or suspicion of repairable nail bed injury), this can be done by separating the nail plate from the nail bed using lifting motions with a hemostat or scissors, being careful to avoid further nail bed damage.
- Nail replacement/nail fold splinting: Replace the nail to preserve nail folds and prevent infection; a recent study (5) has not shown any difference in infection rate or cosmetic outcomes with nail replacement vs sterile dressing. In our experience, replacement of the nail is useful as a biological dressing/splint.
- Injuries and treatment
- Closed injury: nail plate remains in place.
- Even without obvious laceration, if x-rays show a fracture and there is a subungual hematoma present, nail removal and nail bed repair may be indicated. Nail bed repair can be done with dissolvable sutures like 5-0 Vicryl Rapide, or with Dermabond with comparable results (4). Non-adherent gauze should be used as a dressing. See “Nail replacement” above. Any fractures should be splinted for three weeks.
- Open injury without nail bed loss: nail plate is removed exposing injury.
- Suture any obvious lacerations, being careful to maintain as much volar skin attachment as possible to maximize blood flow to the tip. Split/slab any fracture for three weeks.
- Nail bed loss without bone involvement.
- Any loss of nail bed can result in nail deformities. If greater than 1cm consult plastics.
- Nail bed avulsion: Nail bed avulsed from germinal matrix.
- If the nail bed has avulsed along with a fracture it can be reattached to the germinal matrix via pull-through mattress sutures with good results. This will also help with reduction of a distal phalange.
- Amputation
- Pulp only: If patient is younger than two no reattachment is indicated, good outcomes with simple dressing. If over two and the amputated tissue is usable, de-fatting and reattachment is indicated. Otherwise, simple sterile dressing and consideration of plastics referral.
- Pulp and nail/bone: Emergency plastics consultation, wash and dress site of amputation, obtain x-rays. Keep stump covered with moist gauze. Keep severed tissue in an ice water bag, avoid contact with ice.
- Closed injury: nail plate remains in place.
Criteria For Transfer To Another Facility
If requested by consultant.
Ensure any severed tissue is well packaged for transfer. Placed in saline soaked gauze in a plastic bag on ice. Confirm with plastic surgeon.
Criteria For Close Observation And/or Consult
Indications for consultation:
- Plastic surgeons generally see these in outpatient follow up in next few days. Good wound care and moist nonstick dressings are important.
- Hard indications for referral include tendon damage, open dislocation, proximal germinal matrix injuries/avulsion, fingertip amputations with nail/bone involvement.
Criteria For Safe Discharge Home
- Discharge home unless other injuries require admission.
- Discharge instructions include seek medical care if signs of infection or for dressing changes – usually primary care provider.
- Follow-up: For small soft tissue issues or uncomplicated repair of partial amputations or avulsions, or nail bed repair, patients can follow up with their primary care provider in 2-3 days for reassessment.
- For sutured partial amputations or avulsions, or nail bed repair, follow up with plastics in 7 – 10 days.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Expert opinion and experience only.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Richards AM, Crick A, Cole RP. A novel method of securing the nail following nail bed repair. Plast Reconstr Surg [Internet]. 1999;103(7):1983–5. Available from: http://dx.doi.org/10.1097/00006534-199906000-00028
Martin-Playa P, Foo A. Approach to fingertip injuries. Clin Plast Surg [Internet]. 2019;46(3):275–83. Available from: http://dx.doi.org/10.1016/j.cps.2019.02.001
Venkatesh A, Khajuria A, Greig A. Management of pediatric distal fingertip injuries: A systematic literature review. Plast Reconstr Surg Glob Open [Internet]. 2020;8(1):e2595. Available from: http://dx.doi.org/10.1097/GOX.0000000000002595
Strauss EJ, Weil WM, Jordan C, Paksima N. A prospective, randomized, controlled trial of 2-octylcyanoacrylate versus suture repair for nail bed injuries. J Hand Surg Am [Internet]. 2008;33(2):250–3. Available from: http://dx.doi.org/10.1016/j.jhsa.2007.10.008
Jain A, Greig AVH, Jones A, Cooper C, Davies L, Greshon A, et al. Effectiveness of nail bed repair in children with or without replacing the fingernail: NINJA multicentre randomized clinical trial. Br J Surg [Internet]. 2023;110(4):432–8. Available from: http://dx.doi.org/10.1093/bjs/znad031
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 04, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.