Neuromuscular Weakness
Cardinal Presentations / Presenting Problems, Neurological, Toxicology
First 5 Minutes
- In patients presenting with weakness, determine whether or not the weakness represents true neuromuscular weakness or subjective weakness.
- Avoid depolarizing neuromuscular blocking agents if intubation is required in true neuromuscular weakness.
- Critical diagnoses include ischemic and hemorrhagic stroke, Guillain-Barré syndrome, myasthenic crisis and spinal cord compression.
Context
Causes of true neuromuscular weakness originate from disorders of the brain or spinal cord, nerves roots, plexus, or peripheral nerves, neuromuscular junctions or muscle fibers.
Diagnostic Process
Early recognition of signs of impending respiratory failure:
Tachypnea, altered mentation, increased oral secretions, difficulty swallowing, inability to lift head from lying position, weak voice, difficulty speaking, dysarthria, shallow, weak and rapid breathing and accessory muscle use.
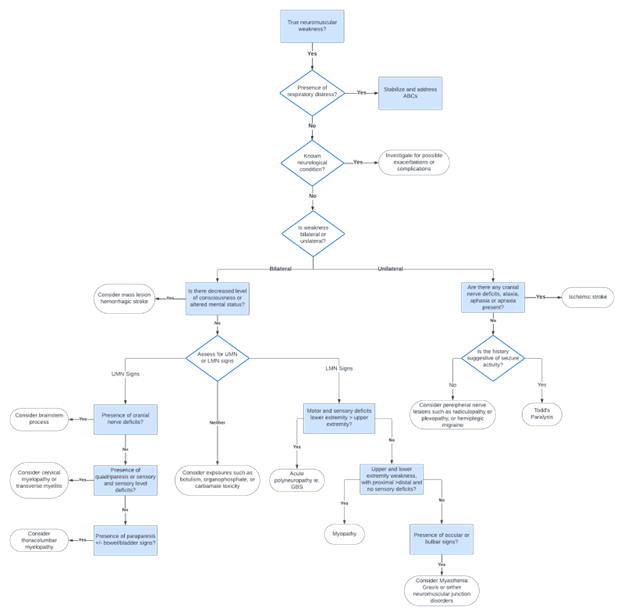
Approach to true neuromuscular weakness in the emergency department. Adapted from various sources.
Investigations:
- ECG
- CBC, BMP, glucose, CK, LFTs, coagulation panel
- +/- neuroimaging as indicated
Recommended Treatment
- Address respiratory failure and intubate as necessary:
- GCS < 8
- Inability to protect airways
- Severe fatigue
- Hypoxemia or hypercarbia
- FVC <12 ml/kg
- Negative inspiratory force <20 cm H20
- Avoid succinylcholine if possible.
- Involve neurology early.
- Treat underlying cause.
- Consult BC poison control if suspected exposure.
Criteria For Hospital Admission
- Decreased level of consciousness.
- Respiratory distress.
- Acute risk of aspiration or inability to protect airway.
Criteria For Transfer To Another Facility
Consult local institutional guidelines.
Criteria For Safe Discharge Home
If careful and thorough assessment has ruled out neurological emergency and rapidly progressive neuromuscular disease, patients may be discharged home with instructions to follow-up with family doctor or specialist as required.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The diagnostic approach is recommended based on robust clinical guidelines and diagnostic features.
Related Information
OTHER RELEVANT INFORMATION
Carpal Tunnel Syndrome : Emergency Care BC
UBC Neurology Clinical Exam Video:
Neurology: Clinical Skills – Motor, Sensory, & Reflex Neurological Exam #neurology #ubcmedicine
Emergency Medicine Cases:
https://emergencymedicinecases.com/approach-acute-motor-weakness/
CanadiEM: https://canadiem.org/crackcast-e201-weakness/
BC Poison Control Toll Free 1-800-567-8911
Reference List
Khamees D, Meurer W. Approach to Acute Weakness. Emerg Med Clin North Am. 2021;39(1):173-180.
https://doi.org/10.1016/j.emc.2020.09.010.
DynaMed. Acute Weakness in Adults – Approach to the Patient. DynaMed. Updated September 22, 2023. Accessed November 22, 2023.
https://www.dynamed.com/approach-to/acute-weakness-in-adults-approach-to-the-patient
Casey KF. Assessment of Acute Motor Deficit. BMJ Best Practices. Updated June 2, 2023. Accessed November 22, 2023.
https://bestpractice.bmj.com/topics/en-gb/1076
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 15, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.