Paroxysmal Supraventricular Tachycardia (PSVT)
Cardiovascular
First 5 Minutes
- Is the patient hemodynamically stable?
- Is the QRS > 0.12 seconds: VT or SVT with aberrancy?
- Is the rhythm regular or irregular?
Context
- Paroxysmal supraventricular tachycardia (PSVT) is characterized by episodic tachycardia with an abrupt onset and resolution.
- PSVT describes atrioventricular nodal re-entry tachycardia (AVNRT), atrioventricular re-entry tachycardia (AVRT) and ectopic/atrial tachycardia (AT). Atrial flutter and atrial fibrillation are discussed elsewhere.
- PSVT is a common presentation in the emergency department for which several treatment options exist1.
- It is important for practitioners to rule out ventricular tachycardia (VT) when diagnosing PSVT.
Diagnostic Process
- Suspect PSVT in all tachycardic patients.
- Standard diagnosis of PSVT requires an ECG. Typical findings include:
- Regular rhythm.
- Narrow QRS complex
- PSVT with aberrancy will present with a wide QRS complex.
- Atypical P wave morphology (absence of P waves or P waves after QRS complex)
- P waves preceding the QRS complex can be seen, causing it to resemble sinus tachycardia.
- Successful treatment of a PSVT with a vagal maneuver or adenosine confirms the diagnosis of PSVT.
- PSVT vs Sinus Tachycardia
- Suggestive of ST:
- A precipitating cause/event is identified.
- The rate varies with respiration or positional changes.
- The rate gradually slows with vagal maneuvers.
- If the heart rate exceeds 220 minus the patient’s age, ST is much less likely.
- Suggestive of ST:
- PSVT vs Atrial Flutter 2:1
- Atrial flutter with 2:1 conduction may present on ECG without characteristic flutter waves, suspicious of atrial flutter with 2:1 conduction if:
- Heart rate is around 150 bpm.
- Flutter wave appears (atrial flutter may briefly conduct as 3:1 instead of 2:1, uncovering flutter waves).
- Vagal maneuvers or adenosine treatment uncover flutter waves.
- Atrial flutter with 2:1 conduction may present on ECG without characteristic flutter waves, suspicious of atrial flutter with 2:1 conduction if:
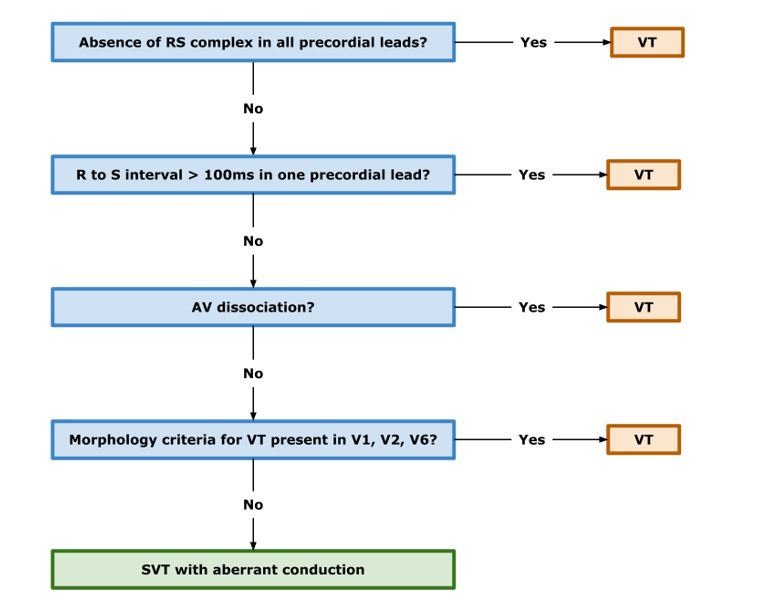
- PSVT + Aberrancy vs VT
- Wide complex PSVT due to accessory pathway or pre-existing bundle branch block may not be readily discernible from VT on ECG. The Brugada criteria was demonstrated to have 90% sensitivity and 64% specificity in a recent meta-analysis.
Recommended Treatment
Acute Management
- Hemodynamically Unstable
- Signs include: altered mental status, significant cardiac chest pain, hypotension (SBP < 90 mmHg), or pulmonary edema.
- Synchronized DC Cardioversion
- Adults | Initial trial at 50 J. If unsuccessful, repeat with 100J.
- Pediatrics | Initial trial at 0.5-1 J/kg. If unsuccessful, repeat with up to 2 J/kg.
Note: Equal efficacy and safety has been demonstrated between biphasic and monophasic cardiac defibrillator monitors. However, biphasic monitors generally require less energy for the same efficacy and should be used if available.
- Hemodynamically StableFirst Line
- Vagal Maneuvers: Valsalva Maneuver
- The modified Valsalva maneuver (REVERT Trial) is shown to have greater efficacy than the standard method (43% vs 17% cardioversion in SVT).
- Patient in a seated position blows into a 10mL syringe for 15 seconds, with just enough force to barely move the plunger.
- Immediately lay the patient supine and lift both legs vertically in the air for another 15 seconds.
- Vagal Maneuvers: Valsalva Maneuver
https://sjrhem.ca/modified-valsalva-maneuver-in-the-treatment-of-svt-revert-trial/
-
- Carotid Sinus Massage (CSM): Auscultate to rule out carotid bruits. Serious neurological effects (0.13%) rare but reported in elderly populations.3
- Adenosine
- Double Syringe Method | 6mg adenosine IV followed by 20mL NS bolus. If unsuccessful, repeat with a second dose of 12mg.
- Single Syringe Method | 6mg adenosine IV diluted with up to 20mL of NS. If unsuccessful, repeat with a second dose of 12mg diluted with up to 20mL of NS.
- A randomized trial from 2022 found moderate quality evidence to suggest no difference in cardioversion success rates between the two methods4. Although underpowered, this study suggests the single syringe method may be useful for clinical scenarios where physical limitations prevent the successful use of the traditional double syringe method.
- Halve dose to 3mg in patients taking dipyridamole or carbamazepine.
- Avoid in patients with 2nd or 3rd degree AV blocks.
- Calcium Channel Blockers (CCBs)
- Diltiazem | 0.25mg/kg IV, increased to 0.35mg/kg IV if unsuccessful.
- Verapamil | 2.5-5mg IV, increased to 5-10mg IV if unsuccessful.
Although AHA guidelines list CCBs as a second-line intervention, moderate-strong evidence suggests CCBs are comparable to adenosine in in efficacy5. Moreover, a number of reports suggest an increased rate of adverse events with adenosine as compared to CCB treatment. Clinicians should not hesitate to use CCBs in place of adenosine when clinical judgement dictates.
Note: Only non-dihydropyridine CCBs possess the cardiac selectivity required to be effective PSVT therapeutics.
-
- Beta-Blockers
- Use in cases of acute PSVT where adenosine/CCBs have failed, or prophylactically for long term prevention of PSVT.
- Adenosine and CCBs are contraindicated in patients with evidence of (VT) or wide complex tachycardia (WCT). Use of these therapeutics in patients where VT and WCT have not been ruled out but may put the patient at risk of becoming hemodynamically unstable.
- Beta-Blockers
Third Line
-
- Synchronized DC Cardioversion
- Reserved for patients who are unresponsive to vagal maneuvers and Adenosine or where VT cannot be ruled out. See above for dosage details.
- Synchronized DC Cardioversion
Long Term Management
- Isolated Episode of PSVT and No Comorbidities
- Follow-up with a family physician. Holter monitoring may be pursued.
- Recurrent PSVT With No Pre-Excitation
- At-home vagal maneuvers are the first line intervention for future events.
- Patients with chronic hypertension may benefit from long-term suppressive therapy using beta-blockers or CCBs.
- Normotensive patients not responding to vagal maneuvers may benefit from a cardiologist referral.
- Recurrent PSVT With Pre-Excitation
- Refer to cardiology for electrophysiology and follow-up. Catheter ablation may be warranted in some of these patients.
Criteria For Hospital Admission
Patients with PSVT will rarely be admitted to hospital unless they remain hemodynamically unstable or develop acute episodes associated with comorbid conditions.
Criteria For Transfer To Another Facility
Transport to another facility is rarely required unless the current facility lacks the necessary resources to manage the unstable patient.
Criteria For Close Observation And/or Consult
Until PSVT is confirmed and resolved, patients should be monitored for changes in hemodynamic stability and complications of potential PSVT mimics, including WCTs and VT.
Criteria For Safe Discharge Home
- Patients may be discharged if they are stable and their episode of PSVT is resolved.
- Discharged patients should be educated on vagal maneuvers that they can try at home during future episodes of PSVT.
- Patients presenting with their first episode of PSVT may follow-up with their family physician.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Modified Valsalva Preferred Over Original Valsalva — Moderate — Has been validated in a large randomized control trial in a single ED setting.
Comparable Efficacy of CCBs and Adenosine — Moderate — Has been validated in a few randomized control trials and systematic reviews in multiple settings.
Related Information
OTHER RELEVANT INFORMATION
Modified Valsalva Maneuver — https://emergencycarebc.ca/clinical_resource/modified-valsalva-manoeuvre-for-supraventricular-tachycardia/
Two Syringe Adenosine Method — https://www.youtube.com/watch?v=WBQrddqWhzo
Reference List
Link MS. Evaluation and Initial Treatment of Supraventricular Tachycardia. NEJM. 2012;367:1438-1448. Available from: https://www.nejm.org/doi/10.1056/NEJMcp1111259?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
Sun X, Teng Y, Mu S, Wang Y, Chen H. Diagnostic accuracy of different ECG-based algorithms in wide QRS complex tachycardia: a systematic review and meta-analysis. BMJ Open. 2023;13e069273. Available from: https://bmjopen.bmj.com/content/13/7/e069273.info
Walsh T, Clinch D, Costelloe A, Moore A, Sheehy T, Watts M et al. Carotid sinus massage — How safe is it? Age and Ageing. 2006;35(5):518-520. Available from: https://academic.oup.com/ageing/article/35/5/518/10005?login=true
Kotruchin P, Chaiyakhan I, Kamonsri P, Chantapoh W, Serewiwattana N, Kaweenattayanon N et al. Comparison between the double-syringe and the single-syringe techniques of adenosine administration for terminating supraventricular tachycardia: A pilot, randomized controlled trial. Clinical Cardiology. 2022;45(5):583-589. Available from: https://onlinelibrary.wiley.com/doi/10.1002/clc.23820
Alabed S, Sabouni A, Providencia R, Atallah E, Qintar M, Chico TJA. Adenosine versus intravenous calcium channel antagonists for supraventricular tachycardia. Cochrane Database of Systematic Reviews. 2017; Issue 10. Art No.: CD005154. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD005154.pub4/full
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 06, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.