Pneumopericardium
Cardiovascular, Respiratory
Context
- Pneumopericardium is a rare occurrence and is characterized by gas (typically air) within the pericardium. It’s causes include a fistula between pericardium and air-containing organ (i.e., stomach, esophagus, bronchi), infectious pericarditis with gas generating organisms, penetrating trauma, thoracic surgery and positive pressure ventilation, severe asthma, respiratory distress syndrome, and procedures (including esophagectomy, endomyocardial biopsy, lung transplantation).
- The pericardium contains the heart and proximal parts of the pulmonary trunk and aorta.
Diagnostic Process
History
- Can be symptomatic or asymptomatic.
- Symptoms include dyspnea and pain over the pre-cardiac region.
Physical Exam
- Although unreliable for detecting pneumopericardium, Bruit de Moulin and Hamman’s Crunch are signs that suggest the pathology.
- Assess for Beck’s Triad (Elevated JVP, muffled heart sounds and hypotension). If presenting with Beck’s Triad, consider tension pneumopericardium, a rare but life-threatening complication of pneumopericardium.
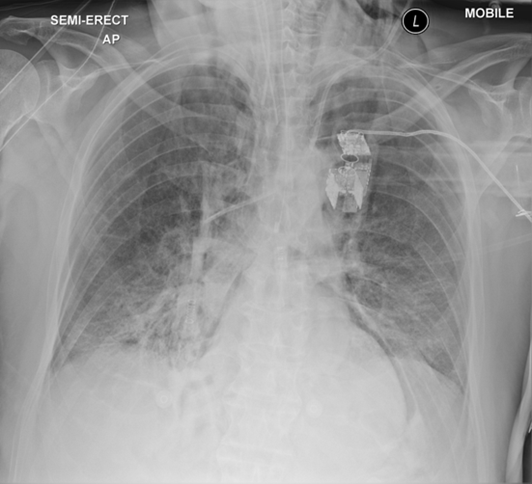
Chest X-ray
- Characterized by a well-demarcated/sharply outlined pericardium that is surrounded by gas.
- Can sometimes see a continuous diaphragm sign. Normally the centre portion of the diaphragm is obscured by the cardiac silhouette, however, if the diaphragm is visualized in the midline, it is suggestive of free gas in the mediastinum or pericardium.
- Pneumopericardium is differentiated from pneumomediastinum in that gas cannot track beyond the anatomical limits of the pericardial sac. Another distinguishing feature between the two is that when the x-ray is taken in the lateral decubitus position, the air will shift immediately in the case of pneumopericardium.
Other Imaging Modalities
- If doing a point of care U/S, it will be more challenging to visualize the heart in the presence of surrounding air, so that could be a diagnostic clue suggesting pneumopericardium. Other findings include bright spots and comet tail artifacts throughout the heart, visualized during diastole.
- If clinically suspecting a pneumopericardium and X-ray is inconclusive, CT scan is the preferred modality.
Recommended Treatment
- Treat the underlying cause.
- Patients can be discharged if asymptomatic and stable. In a simple asymptomatic pneumopericardium, treatment is ongoing surveillance to ensure it doesn’t progress into a tension pneumopericardium.
- Tension pneumopericardium occurs when the build-up in air results in hemodynamic instability. In the event of a tension pneumopericardium, decompression should be done immediately, either by needle pericardiocentesis or placement of a drain. This decision will likely be made in consultation with Cardiothoracics.
- Signs and symptoms of tension pneumopericardium are similar to that of cardiac tamponade and so should be suspected in the event of hemodynamic instability but no visible effusion.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Research is limited to case reports given how rare pneumopericardium is.
Related Information
OTHER RELEVANT INFORMATION
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 10, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.