Procedural Sedation and Analgesia (PSA)
Analgesia / Sedation, Cardinal Presentations / Presenting Problems
Context
The goal is to provide safe, timely and humane care in treating painful conditions and performing painful and/or anxiety-provoking procedures. There are a number of approaches, each with advantages and disadvantages in certain clinical circumstances.
Considerations when choosing PSA
The best choice for PSA depends on the clinical circumstances. Considerations include:
- Procedural factors:
- Sedation depth required;
- Amount of pain associated with procedure;
- Length of the procedure;
- Patient factors:
- Patient’s cardiorespiratory reserve (co-morbid conditions);
- Patient’s anxiety level;
- Fasting status;
- Clinical environment:
- Ability to provide required monitoring;
- The skill set and comfort of available staff with PSA and associated pharmacologic agents
Based on the factors above, clinicians may choose to either proceed with or delay the procedure, consult with additional staff, or consider transfer of the patient to a more appropriate facility.
Contraindications to PSA
Absolute contraindications to PSA:
- Lack of personnel experienced in airway management and advanced life support;
- Lack of familiarity with the medications being used;
- Lack of appropriate monitoring equipment (minimum of continuous cardiac and oxygen saturation monitoring with intermittent BP; end-tidal CO2 recommended if using deep sedation);
- Inability to monitor the patient during the procedure and the recovery period;
- An allergy to relevant medications.
Factors to consider when selecting patients for PSA
- Potential airway compromise:
- Patients with facial / dental / airway factors that might inhibit or preclude bag-mask ventilation or tracheal intubation.
- In this circumstance choose agents with less potential for respiratory depression (e.g., ketamine) and / or sedate to a lighter endpoint. Consider not doing the sedation, or consulting anesthesia colleagues if possible.
- Potential cardiovascular insufficiency:
- Patients with potential cardiovascular complications (elderly/history of heart failure/concurrent serious illness) should be considered for sedation regimens that are less likely to produce hypotension (e.g., ketamine/ketofol).
- Pre-treat with intravenous fluids if not in CHF and consider delay or abandonment of the procedure or consult anesthesia if possible.
- Potential for aspiration:
- No clear relationship demonstrated between fasting status and aspiration.
- Manage the potential risk (i.e. lateral position/gravity with suction).
- While procedures need not be delayed due to unknown or short fasting times, we recommend using brief-acting agents with anti-emetic effects (e.g. propofol or ketofol) rather than agents known to cause emesis (e.g., opiates, ketamine).
- Similar caution should be exercised in patients with ileus, bowel obstruction, and morbid obesity.
Drug Selection
Use what you are most comfortable with – when using a new drug or combination recommend you consult with a colleague who has experience with them if possible.
1. Painful procedures
- Choose a regimen with strong analgesia as well as sedation (e.g. ketofol or ketamine), particularly if there will be pain after the procedure (e.g. fracture reduction, I+D).
- If using propofol alone you should administer an analgesic unless the procedure is particularly short (e.g. cardioversion).
- Opiates in conjunction with propofol lead to more respiratory adverse events.
- Ketamine can provide analgesia with no increased respiratory depression.
2. Short recovery
- Choose shorter-acting agents such as propofol or ketofol (separate syringes or 20:80 / 30:70 mixtures to limit the amount of ketamine given).
- Advantageous where fasting may be inadequate or when personnel and space resources are in demand.
- Etomidate is also an effective option.
3. Post procedure agitation
- In patients with a known history of psychosis, or those with extreme anxiety it may be prudent to avoid the use of ketamine and ketofol as they are associated with more psychomimetic effects than propofol alone.
- Alternatively, be prepared to provide a small dose of midazolam (e.g. 2mg IV in an adult) if necessary.
- Fentanyl / Midazolam Combination: an effective option if there are no concerns regarding airway compromise or prolonged recovery.
4. Impaired cardiovascular status
- In older patients or in patients with known history of congestive heart failure, choose a regimen known to support blood pressure (e.g., ketamine or ketofol) and avoid using propofol alone.
5. Other drug regimens
- Etomidate: This can be used effectively but myoclonus is often a problem. For this reason, it is considered an inferior option to propofol or ketofol.
- Fentanyl / Midazolam Combination: an effective combination but increased respiratory adverse events and prolonged recovery time.
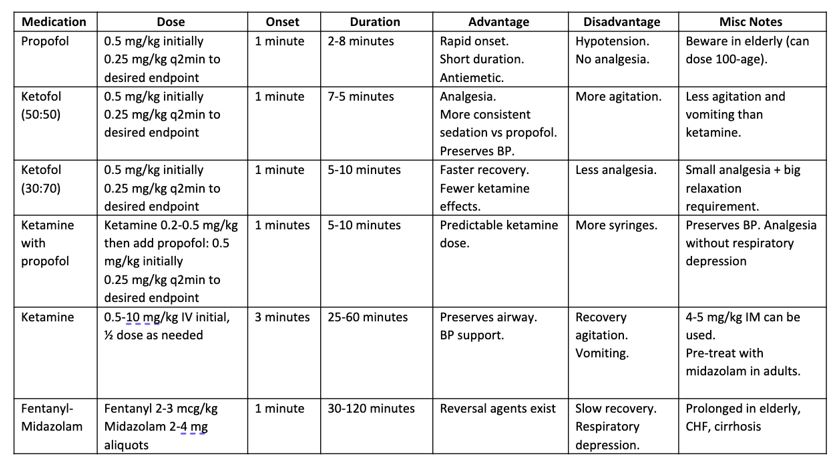
Recommended Drug IV Dosages
Created By Ella Barrett-Chan, MSI UBC
Special Circumstances
Capnography
Capnography can be very handy with limited resources as it improves the detection of respiratory depression and apnea. Many clinicians find this advantageous however clinical outcomes are equally excellent with close clinical observation as outcomes are most dependent on clinical vigilance rather than technology.
High-Risk Patients
Be extremely cautious in the very young and the very old, as well as those with relevant co-morbid conditions (e.g. cardiorespiratory disease, morbid obesity).
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Propofol – High quality evidence; multiple randomized controlled trials
Ketofol – High-quality evidence; several randomized controlled trials
Capnography – Medium evidence for early detection of respiratory adverse events. No evidence for improved clinical outcomes.
Fasting – Low-quality evidence. Expert consensus guidelines exist. No evidence for fasting reducing adverse events.
Related Information
OTHER RELEVANT INFORMATION
Podcast by Dr Andolfatto on ketamine use (NursEM) Part One discusses dosing, myths, pain control and procedural sedation (33:34).
Part Two discusses intubation, behavioural control, physiologic effects and other important info (34:49).
-
-
-
Procedural sedation checklist (EMCrit)
Relevant Resources
RELEVANT RESEARCH IN BC
Procedural Sedation and AnalgesiaRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 16, 2018
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.