Rapid Sequence Intubation
Critical Care / Resuscitation
Context
- Rapid sequence intubation (RSI) is the technique of choice for emergency intubations given that most patients in the ED are at risk of aspiration.
- RSI produces rapid unconsciousness and muscle paralysis to create an optimal condition for laryngoscopy and endotracheal intubation.
Recommended Treatment
RSI steps
- Preparation & planning (Refer to RSI checklist)
-
- Assess for difficulty of intubation and create a plan for airway management. Have an alternative rescue technique.
- Prepare equipment and drugs (SOAP ME)
Suction
Oxygen: BMV
Airway: laryngoscope, ETT, stylet, OPA, NPA, LMA, bougie
Pharmacological: induction agent, paralytic, vasopressors
Monitoring
Equipment: ETCO2, SpO2, ECG, NIBP
- Preoxygenation increases safe apnea time (~8 min in a healthy 70kg adult)
-
- 100% FiO2 for 3-5 min using a non-rebreather mask (NRM) at a flow rate greater than 40L/min while patient is sitting up or in reverse Trendelenburg.
- Consider apneic oxygenation by placing nasal prongs underneath the NRM. Apneic oxygenation has been shown to increase safe apnea time in obese patients and reduce incidence of hypoxemia during RSI.
- Consider non-invasive positive pressure ventilation for hypoxemic or morbidly obese patients.
- Induction followed by paralysis
-
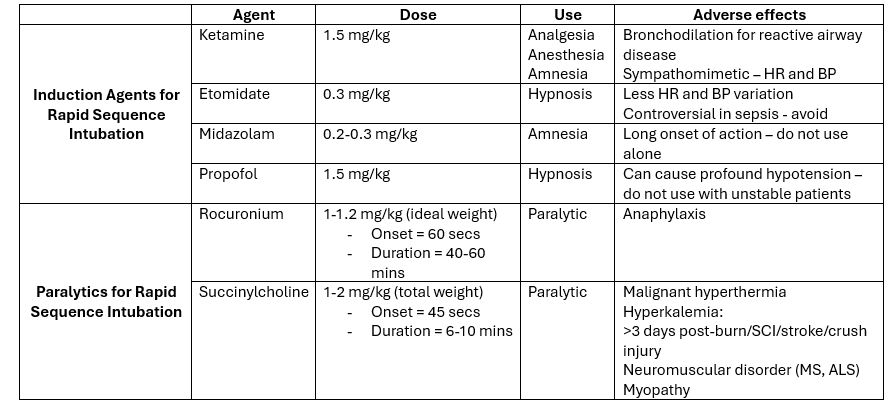
- Ketamine is preferred for induction in hemodynamically unstable patients (table 1).
- All induction agents are direct myocardial depressants. Be prepared to treat hypotension with vasopressors.
- There is a shift towards rocuronium given succinylcholine’s multiple contraindications (table 2). Wait 45 seconds after succinylcholine or 60 seconds after rocuronium administration prior to laryngoscopy.
- Endotracheal intubation
-
- Video laryngoscopy is quickly becoming the preferred intubation device.
- Once oxygen saturation drops below 93%, resume BMV to oxygenate and optimize the plan before re-attempting intubation.
- External laryngeal manipulation (BURP maneuver) may improve visualization of glottis.
- No evidence of cricoid pressure reducing the risk of aspiration. Cricoid pressure has also been shown to increase the difficulty of tracheal intubation.
- Confirmation of ETT placement
-
- Direct visualization of ETT passing through vocal cords
- Confirm chest rise.
- End tidal CO2 monitoring.
- Post-intubation management
-
- Mechanical ventilation.
- Analgesia and sedation.
- CXR to confirm ETT position.
Pearls and pitfalls
- Common ED delivery methods with lower oxygen flow rates will not deliver 100% FiO2 and thus will not adequately pre-oxygenate prior to RSI.
- Ketamine can cause hypotension at doses greater than 1.5mg/kg or in patients that are catecholamine deplete from their underlying disease.
- TBI is not a contraindication for ketamine as it has not been shown to increase ICP.
- Succinylcholine will not wear off fast enough to prevent harm in CICO.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Ketamine as induction agent for unstable patients – high quality evidence. Multiple randomized controlled trials.
Rocuronium – high quality evidence. Multiple randomized controlled trials show similar intubating conditions to succinylcholine.
Preoxygenation with flush rate oxygen and NRM – Moderate quality evidence. Few small randomized controlled trials showing noninferiority to BVM.
Apneic oxygenation – moderate quality evidence. Few small randomized controlled trials showing increased safe apnea time in obese patients.
Ketamine and traumatic brain injury – low quality evidence. Early studies claiming increase in ICP with ketamine has major flaws.
Role of etomidate in sepsis mortality – low quality evidence. Literature is divided and no large RCT has been performed.
Related Information
Reference List
Driver BE, Prekker ME, Kornas RL, et al. Flush rate oxygen for emergency airway preoxygenation. Ann Emerg Med. 2017;69:1–6.
Sakles JC, Mosier JM, Patanwala AE, et al. First pass success without hypoxemia is increased with the use of apneic oxygenation during RSI in the emergency department. Acad Emerg Med. 2016;23:703–710.
Birenbaum A, Hajage D, Roche S, Ntouba A, Eurin M, Cuvillon P, Rohn A, Compere V, Benhamou D, Biais M, Menut R, Benachi S, Lenfant F, Riou B; IRIS Investigators Group. Effect of Cricoid Pressure Compared With a Sham Procedure in the Rapid Sequence Induction of Anesthesia: The IRIS Randomized Clinical Trial. JAMA Surg. 2019 Jan 1;154(1):9-17. doi: 10.1001/jamasurg.2018.3577. Erratum in: JAMA Surg. 2019 Jan 1;154(1):96. PMID: 30347104; PMCID: PMC6439856.
Jabre P, Combes X, Lapostolle F, et al. Etomidate versus ketamine for rapid sequence intubation in acutely ill patients: a multicentre randomised controlled trial. Lancet. 2009;374(9686):293–300.
Chang, Lee C., et al. “The emerging use of ketamine for anesthesia and sedation in traumatic brain injuries.” CNS neuroscience & therapeutics 19.6 (2013): 390-395.
Tran DTT, Newton EK, Mount VAH, et al. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2015;(10):CD002788. doi:10.1002/14651858.CD002788.pub3
Related Information
OTHER RELEVANT INFORMATION
Recommended URLs
https://litfl.com/wp-content/uploads/2019/03/Rapid-sequence-induction-RSI-checklist-GD.pdf
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 19, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.