Rheumatoid Arthritis – Diagnosis, Management, and ED Complications
Inflammatory
Context
- Rheumatoid arthritis (RA) is a chronic, system autoimmune disorder that presents primarily as a polyarticular inflammatory arthritis but may also manifest with extraarticular features.
- If left uncontrolled, the disease leads to destruction of joints due to erosion of cartilage and bone, leading to joint deformities that begin in the periphery and progress to proximal joints.
- The diagnosis of RA is clinical, and should be considered in patients with symmetrical polyarthralgia, joint stiffness, and/or synovitis lasting more than 6 weeks.
- Although the disease itself is not fatal, complications of the disease make it the most common rheumatic disease requiring ICU admission.
- Complications include: atlanto-axial subluxation, cricoarytenoid arthritis, interstitial pulmonary fibrosis, accelerated coronary atherosclerosis, septic arthritis, Felty’s syndrome (triad of RA, splenomegaly and neutropenia), renal failure, and GI hemorrhage amongst many others.
Diagnostic Process
Initial Clinical Presentation
- Insidious in onset with predominant symptoms being pain, stiffness, and swelling of many joints.
- Early typical presentations involve symmetric synovial joint involvement affecting the MCP and PIP joints with sparing of the DIP.
- Morning stiffness or stiffness after a prolonged period of inactivity.
Evaluation
1. History
- Joint involvement, characteristics.
- Morning stiffness (often > 30 min) that usually improves with activity.
2. Physical Exam
- Articular manifestations
- Symmetrical, polyarticular arthritis often involving MCP, PIP, wrists, knees, but sparing the DIP, CMC, and axial skeleton (except for C-spine).
- Joint deformities: Swan neck deformity, Boutonniere deformity, hitchhiker thumb, ulnar deviation of fingers.
- Extraarticular manifestations
- Constitutional symptoms: low-grade fever, myalgia, malaise, fatigue, weight loss, night sweats.
- Rheumatoid nodules.
- Lungs: pleuritis, pleural effusions, interstitial lung disease.
- Eye: keratoconjunctivitis, scleritis, episcleritis.
- Hematological: anemia, neutropenia, splenomegaly, lymphoma.
- Heart: pericarditis, myocarditis.
- Vascular: vasculitis, purpura, livedo reticularis.
3. Investigations
- CRP or ESR.
- CBC.
- Thyroid function tests – autoimmune thyroid disorder is common in patients with RA.
- Serology: ANA, ACPA, RF – note serological studies may be negative (e.g., seronegative RA).
- Synovial fluid analysis – if suspicious of septic arthritis or to exclude other diagnoses.
4. Imaging
- X-ray: recommended as the initial test to assess joint disease severity.
- Ultrasound: utility in assessing synovitis and joint effusion.
- MRI: consider if cervical spine involvement suspected (e.g., atlantoaxial subluxation).
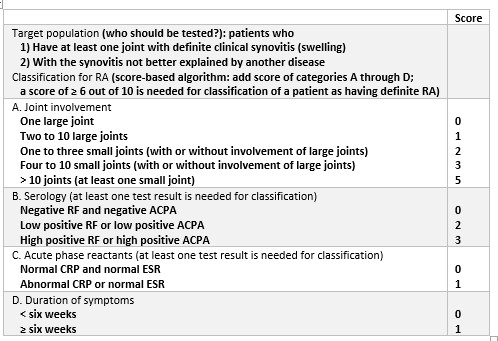
Diagnostic Criteria
The 2010 American College of Rheumatology/European League Against Rheumatism Classification Criteria for RA.
Management
ED Treatment of Acute Flares
Temporary (< 3 months) symptomatic treatment with glucocorticoids and/or NSAIDs.
First line: NSAIDs and selective COX-2 inhibitors
- Ibuprofen, diclofenac, celecoxib.
- No agents have superior efficacy.
- Trial one for 4 weeks at high doses, switch to a different class for 4 weeks.
Second line: Glucocorticoids
- Methylprednisolone 2-32 mg PO daily, 1 to 4-week taper.
- Prednisone 5-10 mg PO daily, 4-week taper.
Long-term pharmacological treatment
Disease modifying anti-rheumatic drugs (DMARDs)
- Methotrexate, hydroxychloroquine, sulfasalazine, tofacitinib.
Complications
Airway
RA causes chronic structural changes to the cervical spine and airway which can increase risk of airway complications.
Atlanto-axial subluxation
- Clinical features: new occipital pain, extremity paresthesias, sensory disturbances, weakness of upper extremities, vertigo, focal neurological deficits.
- Airway management
- Avoid neck hyperextension, even in the absence of symptoms.
- In-line mobilization should be maintained, and fiberoptics or video laryngoscopy.
- Ensure preparation for emergent cricothyrotomy.
- NOTE: DO NOT passively flex or hyperextend the neck of patients with RA as subluxation may be clinically silent.
Cricoarytenoid arthritis
- Clinical features: hoarseness, foreign body sensation, dysphagia, vocal changes, stridor, cough, wheeze, tenderness over cartilaginous structures.
- Airway management
- Ensure preparation for difficult airway and emergent cricothyrotomy.
- Treatment
- High-dose IV methylprednisolone 250-500 mg.
Tracheomalacia
- Airway management
- Smaller than normal endotracheal tube size to avoid cartilaginous destruction.
Pulmonary
Interstitial lung disease and pulmonary fibrosis
- Clinical features: insidious onset cough and exertional dyspnea. Severe cases may lead to pulmonary hypertension and cor pulmonale.
- Imaging shows diffuse infiltrates and PFTs reveal restrictive lung pattern.
- Treatment
- High-dose IV methylprednisolone 1 mg/kg/day for 3 days followed by oral prednisolone 1 mg/kg/day until symptoms improve.
Pleuritis
- Clinical features: dyspnea, pleuritic chest pain, pleural effusions, or friction rub.
- Diagnosis: diagnostic and therapeutic thoracentesis to prevent scarring or fibrosis.
Alveolar hemorrhage
- Clinical features: massive hemoptysis.
- Management: early bronchoscopy, high-dose IV methylprednisolone up to 500 mg q6h, and consideration of tranexamic acid.
Cardiovascular
Accelerated coronary atherosclerosis
- RA patients are at a three-fold increased risk for myocardial infarctions compared to the general population.
- These patients often present with atypical chest pain that is attributed to arthritis, leading to missed MIs and significant morbidity and mortality.
Musculoskeletal
Septic arthritis
- Septic arthritis can easily missed as symptoms are attributed to RA flare.
- Diagnostic arthrocentesis should be performed if there is clinical suspicion.
Hematological
Felty syndrome
- Triad: neutropenia, splenomegaly, and rheumatoid arthritis.
- Patients require thorough evaluation for infection given risk for recurrent and fulminant bacterial infections.
Renal
Renal failure
- RA patients are at increased risk of renal failure secondary to nephritis, rhabdomyolysis, renal vein thrombosis, and fulminant renal failure.
- New onset acute kidney injury should prompt further investigation and early involvement of nephrology and rheumatology.
- Diagnostics include urinalysis and electrolytes however, definitive diagnosis is made via renal biopsy.
Related Information
Reference List
Slobodin, G., Hussein, A., Rozenbaum, M., & Rosner, I. (2006). The emergency room in systemic rheumatic diseases. Emergency medicine journal, 23(9), 667-671.
Dumusc, A., & So, A. (2014). Complications and systemic manifestations of rheumatoid arthritis. Revue Medicale Suisse, 10(421), 590-592.
Berman, S., Bucher, J., Koyfman, A., & Long, B. J. (2018). Emergent complications of rheumatoid arthritis. The Journal of Emergency Medicine, 55(5), 647-658.
Wasserman, A. (2011). Diagnosis and management of rheumatoid arthritis. American family physician, 84(11), 1245-1252.
Aletaha, D., Neogi, T., Silman, A. J., Funovits, J., Felson, D. T., Bingham III, C. O., … & Hawker, G. (2010). 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis & rheumatism, 62(9), 2569-2581.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 08, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.