Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) – Diagnosis
Critical Care / Resuscitation, Ears, Eyes, Nose, and Throat, Inflammatory
Context
- Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) are severe life-threatening Type IV hypersensitivity mucocutaneous reactions characterized by extensive skin detachment and necrosis.
- SJS/TEN are variants of the same disease process and are distinguished primarily based upon the percentage of body surface area (BSA) affected.
- SJS: < 10% skin detachment
- SJS/TEN overlap syndrome: 10-30% skin detachment
- TEN: >30% skin detachment
- SJS/TEN is extremely rare with 1-2 cases/million people per year and can occur at any age, affecting females twice as much as males.
- The mortality rate is approximately 10% for SJS and 50% for TEN.
- Risk factors include HIV infection, immunodeficiency, malignancy (especially hematologic), Lupus, radiotherapy, UV light, or exposure to a new medication 5-56 days ago.
- Re-epithelialization occurs over several weeks, however, the role of hospitalization is a stabilization of the acute phase of SJS/TEN which lasts 8-12 days.
- Emergency physicians have an important role to play in the early detection of SJS/TEN, as early detection and withdrawal of the offending agent greatly improves mortality/morbidity.
- Features suggestive of SJS/TEN:
- Painful rash with erythematous macules.
- Targetoid lesions or diffuse erythema leading to vesicles/bullae.
- Prodrome of febrile illness and cold symptoms (rhinorrhea, cough, conjunctivitis, dysphagia).
- Oral/ocular and/or genital mucosa involvement with painful mucosal erosions.
- Positive Nikolsky sign or necrosis/sloughing of the epidermis.
- New drug(s) started within the past 1-4 weeks.
Diagnostic Process
- There are no formal diagnostic criteria for SJS/TEN.
- SJS may start as a febrile illness with malaise, headache, cough, and/or rhinorrhea 1-3 days before skin lesions appear. Signs of early mucosal involvement include photophobia, conjunctival itching, burning, and dysphagia. Other features include myalgia and/or arthralgia with target lesions.
- Subsequently, skin lesions appear on the face/thorax and are symmetric, ill-defined, coalescing, erythematous macules with purpuric centers. The skin may be tender to touch, with pain out of proportion to findings. These macules progress to vesicles/bullae, which slough off with slight pressure (denouement). The scalp, palms, and soles of feet are usually spared but may be the early site for lesions.
- SJS/TEN affects the oral, ocular, and/or urogenital mucosa in 90% of cases.
- Oral – lesions of the mucosa/vermillion border.
- Ocular – conjunctivitis with purulent discharge, uveitis, corneal ulceration, panophthalmitis, pain, photophobia.
- Urogenital – urethritis in 2/3rds of patients, genital erosions, erosive/ulcerative vaginitis, vulvar bullae, vaginal synechiae (adhesions).
- Chronic urogenital complications include: labial/vaginal adhesions/stenosis, obstructed urinary stream, urinary retention, recurrent cystitis, hematocolpos, vulvovaginal adenosis.
- Other mucosal sites of involvement include the pharynx, trachea, bronchi, and esophageal membranes.
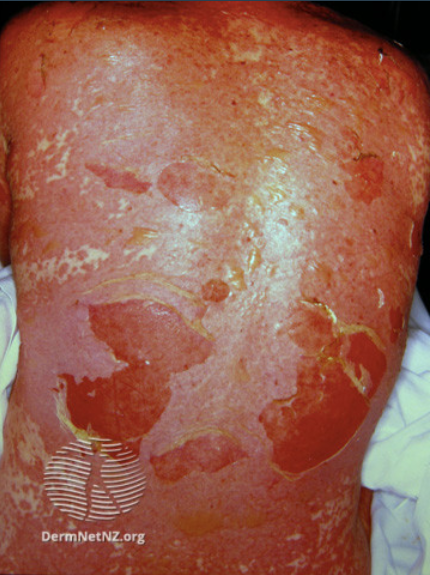
Figure 1. Epidermal detachment of the back in TEN – Image accessed from DermNet NZ.

Figure 2. Oral involvement in SJS/TEN – Image accessed from DermNet NZ.
- New medications started within 5 days to 4 weeks of symptom onset are the leading trigger of SJS/TEN.
- The ALDEN algorithm can be used for a quick assessment of drug causality, especially for patients with more than one drug exposure.
- Each drug is scored from -11 to 10, based on 6 parameters:
- Time from the initial intake of drug to onset of reaction.
- The probability of the drug’s presence on the index day.
- Previous history of exposure (with or without reaction) to the drug.
- Drug presence after the progression phase of the disease.
- The drug known as a cause for SJS/TEN.
- +/- the existence of other etiologies.
- Drugs associated with SJS/TEN in decreasing order of case numbers used in the European Registry.
- Allopurinol
- Lamotrigine
- Sulfamethoxazole
- Carbamazepine
- Phenytoin
- Nevirapine
- Sulfasalazine
- Other sulfonamides
- Oxicam NSAIDs
- Phenobarbital
- Etoricoxib
- Diclofenac
- Doxycycline
- Amoxicillin/ampicillin
- Ciprofloxacin
- Levofloxacin
- Amifostine
- Oxcarbazepine
- Rifampin (rifampicin)
- Infections by Mycoplasma pneumoniae, cytomegalovirus, HSV and hepatitis A have also been linked with some cases of SJS/TEN.
- The differential diagnosis includes other drug eruptions (DRESS, AGEP, Exanthematous drug eruption, fixed drug eruption, lichenoid drug eruption, acneiform eruption secondary to epidermal growth factor receptor), Staphylococcus Scalded Skin Syndrome (SSSS), Kawasaki disease, and erythema multiforme.
- Physical examination should include:
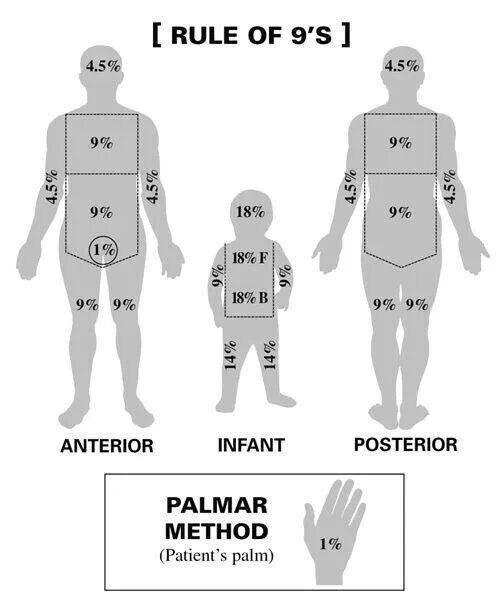
- Approximation of the total affected BSA via the rule of nines (Parkland Formula for Burns).
Figure 3. Estimating BSA affected. Image accessed from Medictests.com
- Positive Nikolsky skin – ability to extend sloughing by pushing laterally on the surface of the skin.
- Positive Asboe-Hansen sign – extending a blister by pushing laterally on the surface of affected skin into unaffected skin.
- Investigations to order:
- CBC + differential, glucose, extended electrolytes, BUN, Creatinine, total protein, albumin, alkaline phosphatase, ALT, AST, ESR or CRP.
- Investigations may reveal non-specific findings such as anemia, lymphopenia, neutropenia, and low albumin. AST, BUN and glucose may be elevated.
- Skin biopsy for Histopathologic analysis should be obtained via a large punch biopsy or deep shave biopsy.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Sensitivity/Specificity of Nikolsky Sign:
Nikolsky sign has a high specificity for detecting damage at the epidermal-dermal junction.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Relevant Resources

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Apr 21, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.