Role of the ED Team in Organ Donation
Administration and Operational Issues, Cardiovascular, Critical Care / Resuscitation, Special Populations, Trauma
Context
- There is a mismatch of supply and demand, with many patients dying waiting for transplant. CIHI data suggest that there are over Canadians waiting for an organ transplant. 260 patients die waiting on the transplant list every year
- Neurologic Determination of Death (NDD) vs Circulatory Determination of Death (DCD)
- Including DCD in end-of-life care process is patient-centered and can save lives
- There is good evidence that referrals from the ED increase the rate of consent and organ donation. A study of 7,000 donor referrals to identify factors associated with successful organ retrieval showed that even after controlling for potential confounders with multiple logistic regression, referral from the ED remained significantly associated with consent granted and with successful organ retrieval.
- However, in Canada, up to 84% of NDD and 46.2% of DCD patients were missed eligible organ donors from the ED.
- One of the hardest things we do is helplessly bear witness to death and devastating injury. If the most we can do is honour a patient’s loss of life by initiating the process of organ donation, then that still counts as good patient care.
Diagnostic Process
- There is usually no reliable way to prognosticate neurologic recovery after cardiac arrest in the ED.
Emergency Physician Role
- Identify and ensure timely referral to BC Transplant for all impending or potential deaths (especially < 75 years) – Tissue Gift Act of BC.
- Under the Human Tissue Gift Act of British Columbia, any impending death (or immediately in the event of death) of a patient 75 years of age or younger that occurs in any hospital in BC, is required to be reported to the Organ Donor Referral Line (1-877-DONOR-BC).
- It is NOT your responsibility to decide if the patient is a suitable organ donor or not.
- Call BC Transplant to ensure your patient receives good patient care, including EOL care.
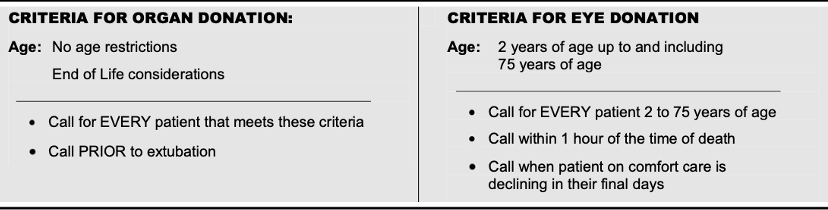
- Introduce organ donation in select scenarios (box below).
- Use family questions as a bridge to introducing the BC Transplant Organ Donation specialist (available 24/7).
- KEEP IT SIMPLE! Don’t worry about knowing the inclusion/exclusion criteria in the ED. Don’t worry about the specifics of neuroprognostication.
- Note: cornea donation is still an option post-arrest for all patients. This is often a big comfort for many families who want their loved one’s life and body to help someone else in need.
- KEEP IT SIMPLE! Allow the experts at BC Transplant to help with discussions and make the decision! Don’t be the gatekeeper to good care – whether that is ongoing resuscitation in the ICU for neuroprotection, neuroprognostication, or organ donation.
Call BC Transplant Early
Calling BC Transplant (available 24/7) early can save you time, aids in the patient’s trajectory, and facilitate timely care.
Why call the BC Transplant Coordinator EARLY on in the dying process? (i.e. why initiate this call from the ED instead of leaving it to the ICU)? There are several reasons:
- BC Transplant can quickly determine if a patient is pre-registered for organ donation – Emergency physicians don’t need to figure out if patients are pre-registered for donation. This is something the BC Transplant team can do which is helpful information to talk through next steps with families.
- BC Transplant can help families explore options. Their team will triage calls and come to help onsite if needed – particularly in tricky cases.
- BC Transplant can help decouple conversations, which is current best practice. Calling early also helps with that concept of decoupling as the BC Transplant team’s highly trained, very skilled team members can approach families before the emergency physician making any major care or disposition decisions.
- Calling BC Transplant will save you time.
- Calling BC Transplant facilitates better patient care! Canadian Consensus Guidelines on best practices reinforce that End of Life Care includes facilitating a patient’s wishes to become an organ donor. In the ED, our first priority is the patient. We must not compromise good EOL care and palliation to enhance the possibility of organ donation. This is why calling BC Transplant allows their team to undertake that potential avenue of care if the family chooses.
Recommended Treatment
5 Steps for the Emergency Physician
1. Identify Potential Donor
Suspected imminent death. This is a patient with a heartbeat in whom you suspect imminent death, whether it’s from an injured brain or non-recoverable injury or medical illness.
2. Ask: Is it the right time to make a referral?
Good EOL care includes the opportunity to GIVE:
- Grave prognosis and/or
- Intention to move towards comfort care
- Ventilated
- Eligibility and registration checked with BC Transplant, ideally before family meeting (call!)
3. Call BC Transplant Coordinator, available 24/7
- Triages calls / May arrive onsite to the ED to assist.
- Quickly check patient’s PHN in Organ Donor Registry.
4. BC Transplant Coordinator
- Screens suitability – updated inclusion and exclusion criteria.
- Approaches family, provides multiple options to make an informed decision.
- Obtains family consent if patient is not pre-registered.
5. Workup for organ donation proceeds in ICU
- NDD OR Controlled DCD with WLSM
Resources
- Call the BC Organ Donor Referral line at 1-877-DONOR-BC.
- Use BC Transplant’s Worksheet – applicable to any hospital in BC.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
These were based on recent 2020 CAEP guidelines and in extensive discussion with leadership at BC Transplant who assisted in the development of this clinical resource.
Related Information
OTHER RELEVANT INFORMATION
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Nov 03, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.