Vaginal Bleeding (>20wks)
Critical Care / Resuscitation, Pregnancy, Special Populations
First 5 Minutes
- Modify resuscitation for physiological changes of pregnancy.
- Circulation: uterine displacement with left lateral decubitus.
- Airway: endotracheal tube 1 size smaller, RSI.
- Breathing: supplemental O2 on all patients.
- Tachycardia and hypotension are late findings of shock in pregnancy and indicate immediate resuscitation with fluids and blood products.
- Do not perform a digital cervical exam without confirming placental location.
- Ongoing maternal and fetal monitoring is critical.
Context
- Associated with increased maternal and fetal mortality.
- Life-threatening causes include placenta previa, vasa previa, placental abruption, uterine rupture, placenta accreta spectrum, and coagulopathy.
- Other causes: cervical trauma, labor (bloody show), cervicitis, cervical polyp.
Diagnostic Process
- Detailed history, U/S to exclude placenta previa, and careful pelvic and abdominal exams are key.
- Differentiate minor bleeding and hemorrhage.
- Minor bleeding can be caused by cervical exam or sexual intercourse as a result of increased tissue friability.
- Bloody show is associated with cervical dilation.
- Hemorrhage classically presents with a sudden gush of bright red blood with or without abdominal pain and cramping.
- Consider if blood loss >50mL.
- Placenta previa: painless vaginal bleeding (+/- known placenta previa).
- Vasa Previa: painless vaginal bleeding with rupture of membranes and fetal distress (bradycardia and sinusoidal wave pattern).
- Placental Abruption: vaginal bleeding associated with severe abdominal and/or back pain +/- uterine fundal tenderness and abnormal uterine contractions.
- More common following trauma.
- Amount of blood does NOT correlate to severity of abruption.
- U/S not sufficiently sensitive to rule out.
- Uterine Rupture: vaginal bleeding, severe abdominal pain, easily palpable fetal body parts, fetal distress.
- Placenta Accreta Spectrum: the placenta does not detach spontaneously. Marked intra-/postpartum hemorrhage after preterm or precipitous labor with prolonged 3rd stage of labor.
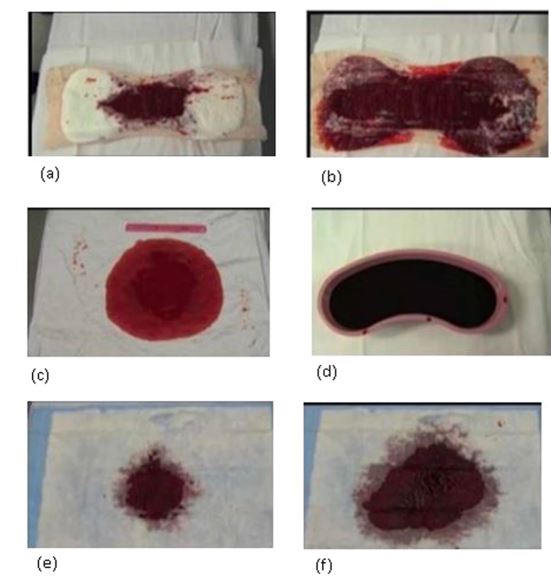
Figure 1. Visual depiction of known blood volumes to aid in blood loss estimation. (a) 100mL (b) 300mL (c) 250mL (d) 500mL (e) 50mL (f) 200mL. Open Access, https://openi.nlm.nih.gov/detailedresult?img=PMC5399603_srep46333-f2&query=obstetric%20hemorrhage%20blood&it=xg&req=4&npos=23 (1).
- Investigations: CBC, blood type/screen and cross-match, fibrinogen, PT/PTT, calcium, magnesium, electrolytes, LFTs.
- Rule-out DIC with blood work; consider HELP.
Recommended Treatment
- Stabilize – Circulation, Airway, Breathing.
- Access: 2 large bore IVs.
- Resuscitate with crystalloid fluids and blood products.
- Activate Massive Transfusion Protocol as appropriate:1:1:1 ratio for pRBCs:platelets:FFP.
- Rhogam for Rh(-) patients.
- Supplemental O2 for all patients.
- ET tube 1 size smaller (ie. 6.0), if required, with RSI.
- Continuous fetal monitoring.
- Tocometry to assess for contractions.
- OB consult.
- Emergency c-section indicated for maternal instability or fetal distress.
- For placenta previa and placental abruption with mild bleeding and hemodynamic stability:
- Labor and delivery for monitoring.
- Vaginal delivery if >34wks with active contractions.
- Betamethasone 12 mg IM if <34wks.
- Magnesium sulfate 4g IV if <34wks.
- Consider tocolysis: terbutaline 0.25mg IM if <34wks and active contractions.
- Placental Abruption – hemorrhage:
- Can result in consumptive coagulopathy, replete clotting factors and fibrinogen if available.
- Uterine Rupture: terbutaline 0.25mg IM to slow contractions, then emergency c-section.
- Placenta Accreta Spectrum: follow institutional PPH guidelines for uterotonics (Postpartum Hemorrhage: Diagnosis and Management : Emergency Care BC).
- Do not apply traction to umbilical cord.
- +/- Interventional Radiology consult if available for uterine artery embolization.
- Surgical maneuvers to prevent blood loss include B-lynch sutures, Bakri balloon inflation, internal iliac artery ligation, interventional radiology embolization, and hysterectomy.
- Maternal DIC Management:
- Avoid hypothermia.
- Platelet transfusion threshold < 50.
- FFP if PT/PTT prolonged.
- Identify underlying cause and treat.
Criteria For Hospital Admission
All but minimal bleeding, except in trauma or anticoagulant use.
Criteria For Transfer To Another Facility
If working in a center without access to OB focus on maternal stabilization and then arrange for immediate transfer to tertiary care for patients presenting with hemorrhage.
Criteria For Close Observation And/or Consult
Patients with non-hemorrhagic bleeding, stable vital signs and reassuring FHR are suitable for observation and expectant management on the labor and delivery ward in the presence of placenta previa and placental abruption.
Criteria For Safe Discharge Home
Minor vaginal bleeding following cervical exam, membrane sweep, or sexual intercourse with no active bleeding, stable vital signs and reassuring FHR are suitable for discharge.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Recommendations based on SOGC Clinical Practice Guidelines and high-quality evidence from emergency medicine textbooks.
Related Information
OTHER RELEVANT INFORMATION
Anti-D Immunoglobulin [RH(D)] : Emergency Care BC
CREOGs Over Coffee 2nd and 3rd Trimester Bleeding:
https://www.podbean.com/ep/pb-fyif4-10af31bCREOGs Over Coffee Placenta Accreta: https://www.podbean.com/ep/pb-bz67c-fc4c87 + https://www.podbean.com/ep/pb-r73jb-fd761c
JOGC Current Clinical Practice Guidelines: https://www.jogc.com/current-guidelines-english
PHSA Clinical Practice Guideline for Massive Hemorrhage: Clinical Practice Guideline
Reference List
Dynin M, Lane DR. Bleeding in Late Pregnancy. In: Borhart J, eds. Emergency Department Management of Obstetrics Complications. 1st ed. Springer, Cham; 2017:53-62. Accessed November 22, 2023.
https://doi.org/10.1007/978-3-319-54410-6_5
Jain V, Bos H, Bujold E. Guideline No. 402: Diagnosis and Management of Placenta Previa. J Obstet Gynaecol Can. 2020; 42(7):906-917.
https://doi.org/10.1016/j.jogc.2019.07.019
Hobson SR, Kingdom JC, Murji A, Windrim RC, Carvalho JCA, Singh SS, et al. Guideline No. 383: Screening, Diagnosis, and Management of Placenta Accreta Spectrum Disorders. J Obstet Gynaecol Can. 2019; 41(7):1035-1049.
https://doi.org/10.1016/j.jogc.2018.12.004
Young JS. Maternal Emergencies After 20 weeks of Pregnancy and in the Peripartum Period. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 9th ed. McGraw Hill; 2020: 6-9. Accessed November 22, 2023.
https://accessmedicine.mhmedical.com/content.aspx?bookid=2353§ionid=219643416
Image Reference:
1.Zuckerwise LC, Pettker C, Illuzzi J, Raab CR, Lipkind HS. Visual aid depicting known volumes of blood on obstetric materials. 2017. Available from: DOI: 10.1097/AOG.0000000000000233. [Accessed November 22, 2023].
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 15, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.