Vaginal Bleeding in Non-Pregnant Patient
Obstetrics and Gynecology
Context
Vaginal bleeding is a common emergency department complaint. Severe vaginal bleeding after pregnancy is excluded, it is less common but can be a sign of occult disease.
Management
The initial management requires stabilization of the patient with blood products, if needed, before further workup is arranged. High dose IV conjugated equine estrogen 25 mg IV q4h x 24 hours is also a first-line option for life-threatening uterine bleeding (7).
Contraindications to estrogen – history of PE or DVT, breast cancer, or liver disease (caution use in patients with CVD due to limited data).
Diagnostic Process
- History and physical exam
a. Pre-menarche
-
- The use of a speculum or attempts to visualize the cervix in the emergency department is often unnecessary.
b. Menarche
-
- Genital and pelvic exams should focus on identifying the source and amount of bleed with the use of a speculum to assess the cervix and vaginal mucosa.
- Bimanual exams should be performed to assess for cervical consistency, uterine position and size, pelvic masses, and cervical motion tenderness.
c. Post-menarche
-
- Genital and pelvic exams should focus on identifying the source and amount of bleed with the use of a speculum to assess the cervix and vaginal mucosa (a Pederson or pediatric speculum may be required if the perineum and external genital is atrophic).
- Bimanual exams should be performed to assess for cervical consistency, uterine position and size, pelvic masses, and cervical motion tenderness.
- CBC, coagulation studies, beta HCG to exclude pregnancy.
- Vaginal cultures for chlamydia and gonorrhea.
- Pelvic – often does not need to be completed in the emergency department unless there is a need to evaluate pelvic pain or rule out a tubo-ovarian abscess.
Note: often the underlying cause is not identified in the emergency department. Emergency physicians are responsible for stabilizing the patient and should have an idea of how urgent follow-up is required so that definitive diagnosis and management occurs.
Pre-menarche (2)
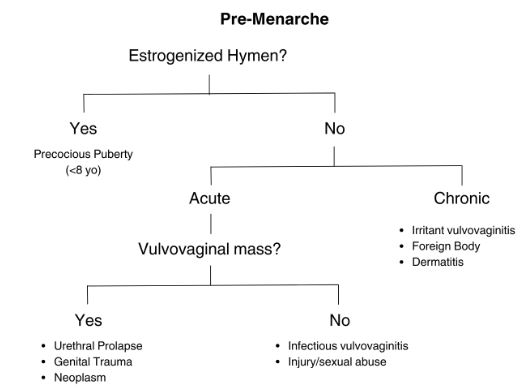
Created by Ella Barrett-Chan, UBC MSI3, 2023
Created by Ella Barrett-Chan, UBC MSI3, 2023
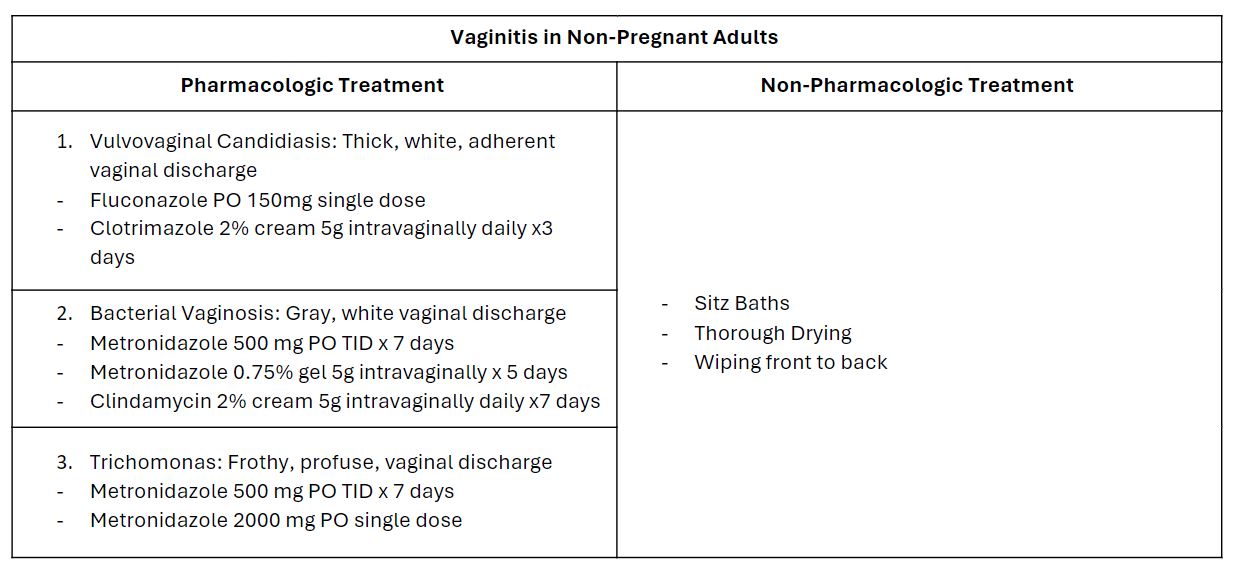
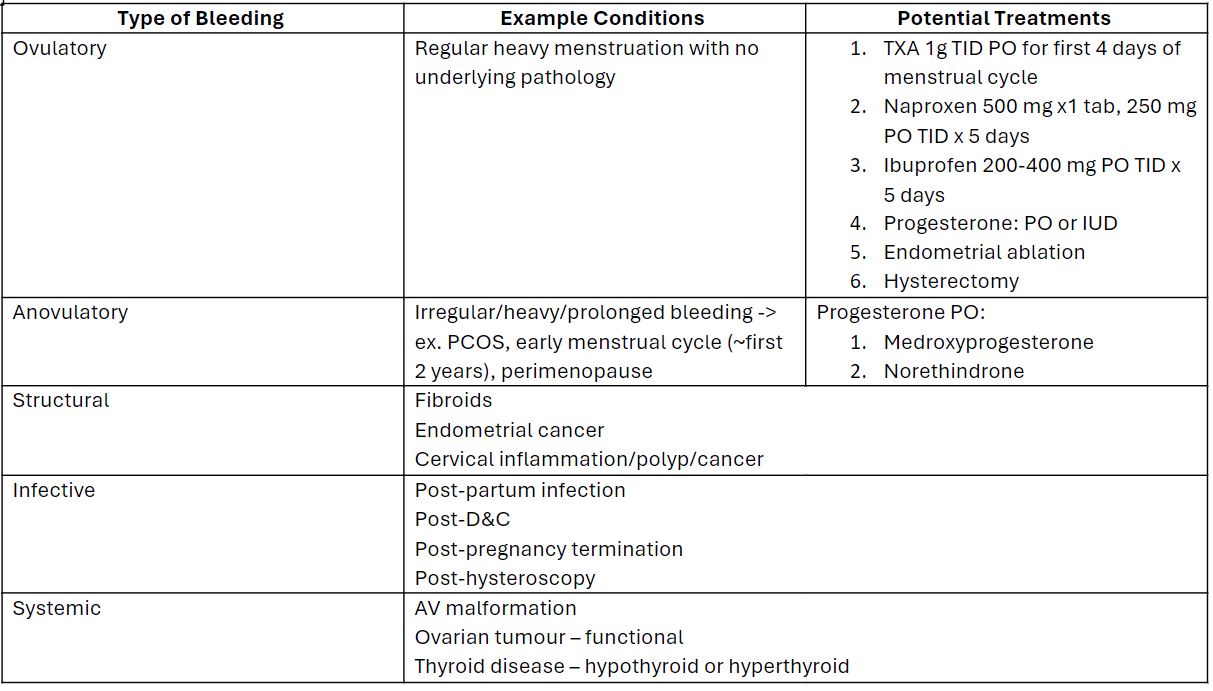
Menarche (3)
Created by Ella Barrett-Chan, UBC MSI3, 2023
Some patients will have underlying coagulopathy or inherited coagulation disorder (heavy bleeding often occurs soon after menarche). Testing for underlying coagulopathy should be considered only in women with a history of heavy menstrual bleeding since menarche or who have a personal or family history of abnormal bleeding.
Diagnosed on ultrasound (endometrial sampling for endometrial carcinoma).
Endocervical samples should be obtained for microscopy and culture to guide treatment (completed by gynecology or some family physicians).
Post-menarche (4)
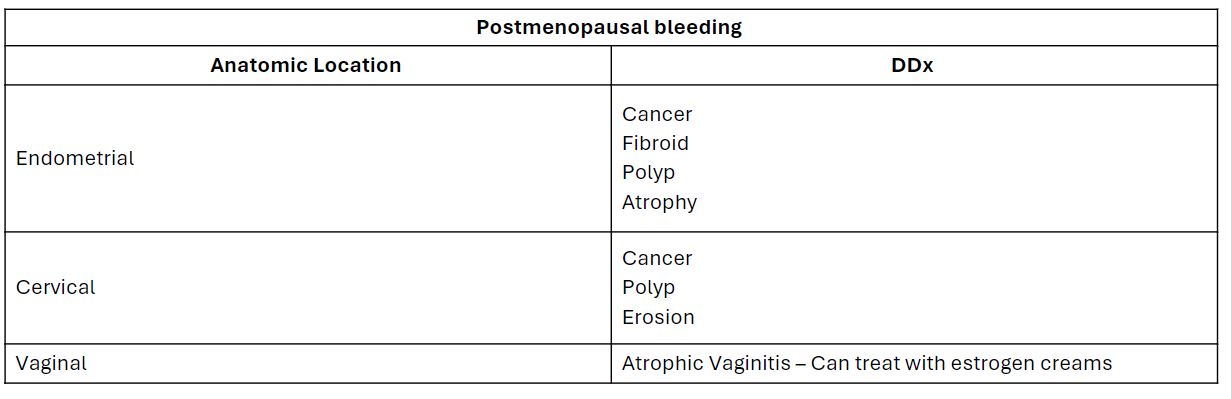
Created by Ella Barrett-Chan, UBC MSI3, 2023
Criteria For Hospital Admission
- Heavy vaginal bleeding with signs of intravascular volume depletion.
- Recent abortion may warrant consultation with a gynecologist due to the risk of retained products.
- Refer to a gynecologist if structural lesion or malignancy is suspected.
- Refer to a gynecologist if medical therapy is inadequate to control bleeding.
- If sexual abuse is suspected, do not discharge a young patient back to the potentially harmful environment.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Recommend behaviour modifications for vaginitis – II-2A.
NSAIDs and antifibrinolytics can treat heavy menstrual bleeds that are cyclic – I-A.
Combined OCPs, depot medroxyprogesterone, and levonorgestrel IUDs reduce menstrual bleeding and can be used to manage abnormal uterine bleeding in patients who also desire effective contraception – I-A.
Assessment of underlying coagulation disorders should be considered only in women with a personal or family history of abnormal bleeding including heavy bleeding beginning at menarche – II-2B.
High-dose estrogen and tranexamic acid may be helpful to manage acute heavy menstrual bleeding – III-C.
Related Information
Reference List
Daniels RV, McCuskey C. Abnormal vaginal bleeding in the nonpregnant patient. Emerg Med Clin N Am. 2003; 21(3): 751-772.
Howell JO, Flowers D. Prepubertal vaginal bleeding: etiology, diagnostic approach, and management. Obstet Gynecol Surv. 2016; 71(4): 231-242.
Bryan S. Abnormal vaginal bleeding. Emerg Med. 2003; 15(3): 215-218.
Birnbaum S. Approach to the woman with abnormal vaginal bleeding. In: Primary care medicine: office evaluation and management of the adult patient. 2014. p. 845-851.
Zuckerman A, Romano M. Clinical Recommendation: Vulvovaginitis. Journal of Pediatric and Adolescent Gynecology. 2016;29(6):673-679. doi:10.1016/j.jpag.2016.08.002
Bofill Rodriguez M, Lethaby A, Farquhar C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database of Systematic Reviews. 2019;9. Art. No.: CD000400. DOI: 10.1002/14651858.CD000400.pub4.
Dyne PL, Miller TA. The patient with non-pregnancy-associated vaginal bleeding. Emerg Med Clin N Am. 2019; 27(2): 153-164. https://doi.org/10.1016/j.emc.2019.01.002
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 24, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.