Acromioclavicular Joint Separation
Orthopedic, Trauma
Context
Most commonly occur with a direct blow to the shoulder. 9-12% of shoulder injuries have Acromioclavicular (AC) joint involvement.
- Peak incidence is ages of 20-29, most commonly males who play contact sports.
- The majority of patients with an isolated, low-grade (Type I-III) AC separation can be discharged home and managed on an outpatient basis.
- Higher grade separations (Type IV-VI) may require surgical repair.
Diagnostic Process
History
- Direct lateral or superior blow to the acromion, usually with the arm in an adducted position.
- Less commonly with a fall on outstretched hand (FOOSH) injury.
- Pain, deformity, or instability over the AC joint, worsened by arm elevation.
Physical
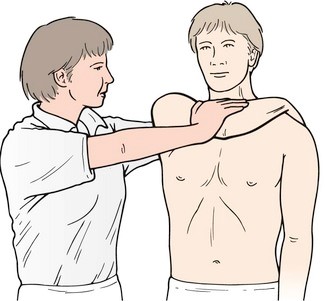
- Rule out brachial plexus involvement – cervical spine screen, distal neurological and vascular examination.
- Rule out injury to associated structures via palpation (Sternoclavicular joint, clavicle, acromion, scapula, coracoid process, humerus).
- Swelling and tenderness located at the AC joint; deformity, prominence or displacement of the clavicle may be noted in higher-grade injuries.
If the injury is mild and diagnosis unclear, special testing can be performed (see Related Information for videos):
-
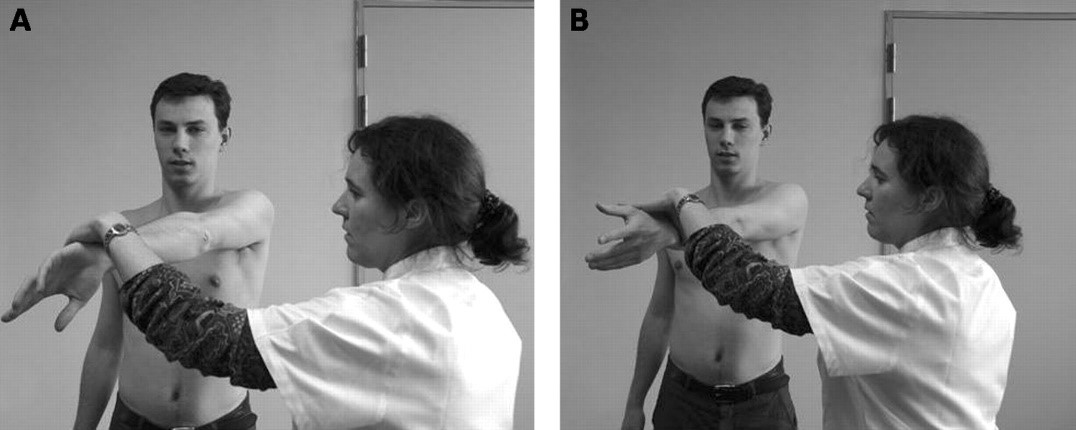
- Cross-body adduction test (77% sensitivity, 79% specificity).
- Passively hold the patient’s straight arm at 90 degrees of shoulder flexion, in neutral rotation; then passively horizontally adduct across the patient’s body.
- A positive test is indicated by the reproduction of pain.
- Cross-body adduction test (77% sensitivity, 79% specificity).
O’Brien (active compression) test (41% sensitivity; 94% specificity).
-
- Instruct patient to flex shoulder to 90 degrees, and horizontally adduct by 10-15 degrees.
- Passively internally rotate the arm maximally, and ask the patient to resist an inferiorly directed force (positive test = provocation of pain).
- Repeat with arm in an externally rotated position (pain should be reduced/absent).
Source: BMJ (https://bjsm.bmj.com/content/42/8/628).
Imaging
Radiographs
- Suspected AC joint injury should initially be evaluated with a plain x-ray.
- Recommend single AP radiograph of both shoulders for maximal detail; arm placed in internal rotation.
- If initial views are non-diagnostic, consider an AP glenoid, or Zanca view: Xray taken with a 10-15 cephalad angle to better demonstrate the acromioclavicular joint free from superimposition.
- An axillary view can be used to rule out coracoid fracture or to confirm clavicle position in Type III-IV separations (see Grading).
- Stress (weighted) views are no longer recommended due to limited diagnostic value and pain.
Other
- Ultrasound or MRI for detailed evaluation are typically ordered on an outpatient basis – not an ED order.
- Evaluation with CT is not recommended.
Grading
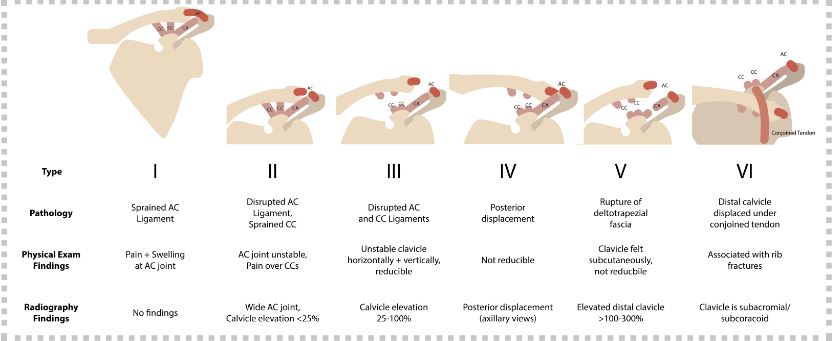
Created by Ella Barrett-Chan, UBC MSI3, 2023
Recommended Treatment
Conservative Management
- Rest, ice, and analgesics PRN.
- Shoulder immobilization (see below for specific recommendations by injury type).
- Shoulder range of motion exercises as soon as tolerated to minimize the risk of adhesive capsulitis.
- Referral to primary care physician and/or physiotherapy for ongoing management.
Management by Injury Type
Type I-II
- Conservative management.
- Sling for <3-7 days.
- Recovery timelines: Type I = 1-2 weeks; Type II = 3-4 weeks.
Type III
- Urgent referral (3-7 days) to orthopedics indicated for consideration of operative repair, though conservative management usually adequate.
- Sling for <2-3 weeks.
- Recovery timeline: 6-12 weeks.
Type IV-VI
- Requires referral for orthopedic evaluation for consideration of operative repair.
- If neurovascular compromise is present, referral should be emergent.
- Prognosis variable.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Low-to-moderate. Management of low-grade and high-grade AC joint injuries have widely consistent management recommendations, but criteria for surgical management is debated.
Related Information
Reference List
Acromioclavicular joint injuries (“separated” shoulder)
Koehler SM. Updated Feb 4, 2021. Accessed Apr 15, 2021.
– UpToDate.Acute Shoulder Injuries in Adults.
Monica J, Vredenburgh Z, Korsh J, et al. 2016;94(2):119-127.
– American Family Physician JournalAcromioclavicular Separation – Emergency Management.
Silverio L. Updated Nov 30, 2018. Accessed Apr 15, 2021.
– Dynamed.Special test links:
The shoulder
Musculoskeletal key
– Musculoskeletal Insight Engine
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 10, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.