Acute Hip Dislocation
Critical Care / Resuscitation, Orthopedic, Trauma
First 5 Minutes
- Dislocations and fracture-dislocations of the hip are true orthopedic emergencies.
- Considerable force is required to produce dislocations and fracture-dislocation; therefore, a hip dislocation serves as a red flag for multisystem injury and should prompt a thorough investigation for other injuries.
- Determine mechanism of injury, assess for other injuries, and perform appropriate resuscitation following ATLS protocols as needed.
- Perform, and document, a detailed neurovascular assessment focusing on sciatic nerve and femoral vessels of affected limb.1,2
- Determine if the patient has a history of a total hip replacement of the affected limb.
Context
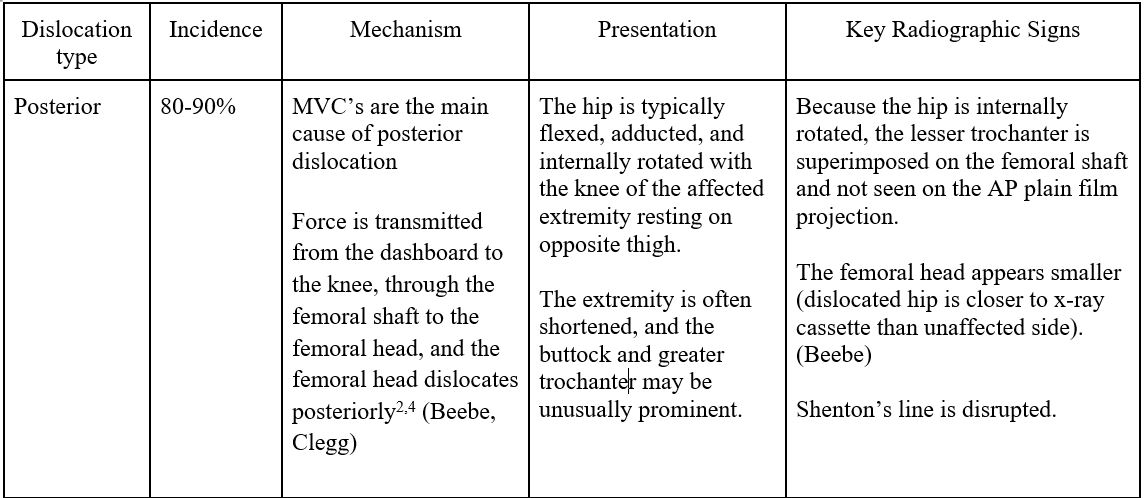
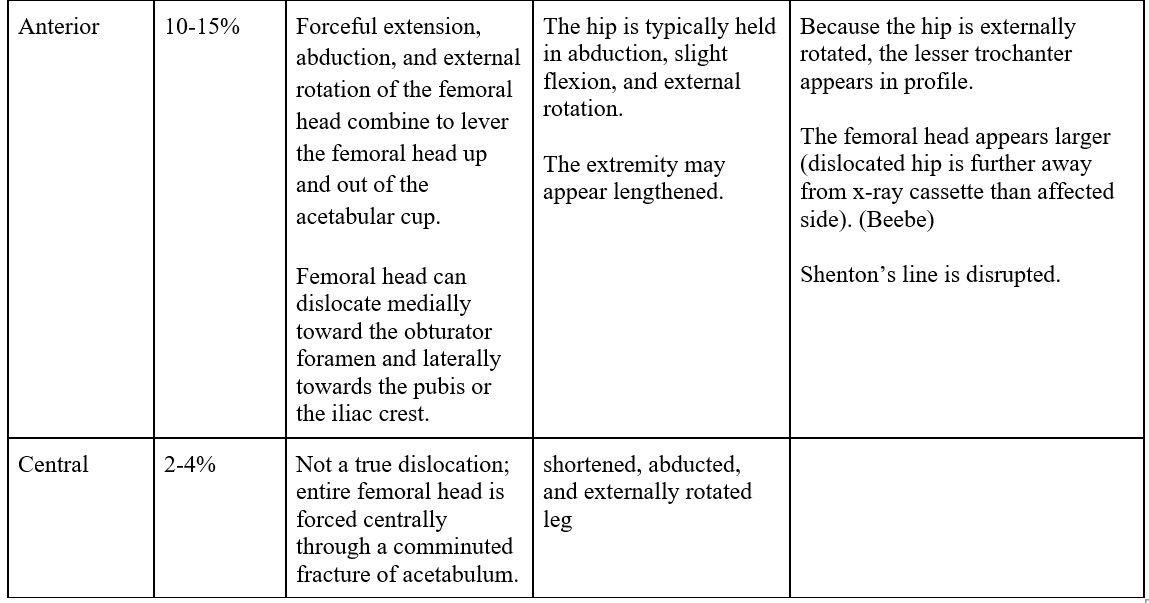
- Hip dislocations are traumatic injuries that result in dislocation of the femoral head from the acetabular socket (90% are posterior).
- Complications:
- Fracture – acetabulum, pelvis, femur.
- Femoral artery/nerve injury (associated with anterior hip dislocation) (Beebe).
- Sciatic nerve injury.
- Avascular Necrosis (AVN).
- AVN develops in 2-10% of patients when reduction is performed within 6 hours3, and in up to 60% of patients when reduction occurs after 12 hours.1
Fracture-dislocations of the Femoral Head
- Femoral head fractures occur in 33-55% of anterior hip dislocations and 10-16% of posterior hip dislocations.1
- Mechanism is typically the result of high-speed vehicular trauma.
Diagnostic Process
Imaging
- AP pelvis and lateral hip plain X-rays are typically adequate for the initial evaluation of hip dislocations +/- femoral neck fractures.3
- Findings suggestive of hip dislocation:
- Disruption of Shenton’s line (arc along inferior femoral neck and superior obturator foramen).
- Disruption of congruence between femoral head and acetabulum.
- Unless there is suspicion for a nondisplaced femoral neck fracture, prioritize emergent reduction prior to CT scan.4
- Obtain CT pelvis following reduction to evaluate for loose bodies, femoral head fracture, or acetabular fracture.
- In the case of irreducible dislocations, a CT scan should be performed emergently to expediate surgical intervention.4
- Findings suggestive of hip dislocation:
Recommended Treatment
Nonoperative:
- Hip dislocations are a true orthopedic emergency and reduction should be performed within 6 hours to reduce the risk of AVN.5,6
- Overall condition of the patient, type of dislocation, and presence (or absence) of associated fractures dictate the timing and method of reduction.
- For simple dislocations, closed reduction should be attempted under procedural sedation. While some clinicians recommend the procedure be performed with the patient under general anesthesia, delays can increase the rate of AVN.
- Closed reduction can produce satisfactory results in most cases.
- If closed reduction is unsuccessful, open reduction is indicated.1
- Relative contraindications to closed reduction include:
- The presence of a femoral neck fracture.
- The presence of other fractures in the ipsilateral extremity.
Reduction Techniques:
- Commonly used reduction techniques include:
- Whistler
- Captain Morgan
- Stimson
- Allis
For full description of these, and other useful hip reduction techniques, please see open access Waddell article referenced in “Related Information” below.
Post reduction:
- Test for stability – gently take hip through its full range of motion to see if it will re-dislocate
- Obtain radiographs (AP pelvis and cross-table lateral hip) to verify adequacy of reduction4:
- Shaft of the femur is in neutral position.
- Shenton’s line is intact.
- Profile of the lesser trochanter is well-visualized.
- Intra-articular space is symmetric and at the same depth as the unaffected joint
- Asymmetry indicates an entrapped intra-articular fragment and is an indication for CT.
- Obtain CT following reduction for evaluation of loose bodies, acetabular fractures, or femoral head fractures.
Dislocation of prosthetic hips
- Management of a dislocated prosthetic hip is similar to native hip dislocation.
- Diagnostic studies and reduction techniques are identical to native hip dislocations, but are not as time-dependent.
- Consultation with an orthopedic surgeon regarding reduction techniques and for development of a long-term treatment plan for the patient (chronic dislocations may require operative repair) is recommended.
Criteria For Hospital Admission
- Most patients with a native hip dislocation require admission to hospital for serial examinations and to ensure no additional injuries are present.
- Patients with fracture-dislocation of the femoral head should be admitted for operative management.
- Multiple traumatic injuries that require inpatient treatment/observation.
- Vascular or neurologic compromise.
- Fracture-dislocations in the elderly that culminate in loss of independence and ability to cope.
Criteria For Transfer To Another Facility
- Indications
- In the case of native hip dislocations, most patients will require urgent orthopedic referral. If onsite consultation is not available, urgent transfer to a referral centre is indicated
- Transport considerations
- Ensure patient has been appropriately resuscitated and is in a stable condition.
- Ensure adequate pain control with appropriate analgesia.
Criteria For Close Observation And/or Consult
- Orthopedic consult is warranted in hip fracture-dislocations or prosthetic hip dislocations.
Criteria For Safe Discharge Home
- Weight bearing as tolerated with crutches for comfort; educate patient on posterior and anterior hip precautions for 6 to 8 weeks (depending on the direction of dislocation); follow up with orthopedics.2
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Hip dislocations are well studied, and resources cited systematic reviews for assessment and management, though reduction technique and surgical management practice patterns are variable.
Related Information
OTHER RELEVANT INFORMATION
Waddell BS, Mohamed S, Glomset JT, Meyer MS. A detailed review of hip reduction maneuvers: a focus on physician safety and introduction of the Waddell technique. Orthopedic Reviews. 2016 Mar 3;8(1).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4821229/
Reference List
Walls, R, editor-in-chief. Rosen’s emergency medicine: concepts and clinical practice. Tenth edition. Philadelphia: Elsevier; 2023
Clegg TE, Roberts CS, Greene JW, Prather BA. Hip dislocations—epidemiology, treatment, and outcomes. Injury. 2010 Apr 1;41(4):329-34.
Tornetta P, Mostafavi HR. Hip dislocation: current treatment regimens. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 1997 Jan 1;5(1):27-36.
Beebe MJ, Bauer JM, Mir HR. Treatment of hip dislocations and associated injuries: current state of care. Orthopedic Clinics. 2016 Jul 1;47(3):527-49.
Dreinhofer KE, Haas NP, Tscherne H. Isolated traumatic dislocation of the hip. Long-term results in 50 patients. The Journal of Bone & Joint Surgery British Volume. 1994 Jan 1;76(1):6-12.
Jaskulka RA, Fischer G, Fenzl G. Dislocation and fracture-dislocation of the hip. The Journal of Bone & Joint Surgery British Volume. 1991 May 1;73(3):465-9.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Mar 13, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.