Angioedema
Cardiovascular, Critical Care / Resuscitation, Ears, Eyes, Nose, and Throat, Gastrointestinal, Inflammatory, Respiratory, Toxicology
First 5 Minutes
If patient is in respiratory distress or presents with hemodynamic instability with angioedema, treat for anaphylaxis and prepare for airway management.
Respiratory distress can occur rapidly and may create a difficult intubation. Get help EARLY, including ED staff, RT, and/or anesthesia/ENT. Surgical airway may be needed in some cases.
There are essentially two distinct types of angioedema based on pathogenesis: histamine mediated and non-histamine (bradykinin) mediated.
Histamine-mediated angioedema should be treated with epinephrine, antihistamine (anti-H1) and steroids.
These medications are not effective for bradykinin mediated angioedema, instead:
- C1 inhibitor protein replacement (berinert, purified C1 inhibitor concentrate, Fresh frozen plasma).
- Kallikrein inhibitor, ecallantide (not currently licensed in Canada but may be requested through the Special Access Program of Health Canada).
- Bradykinin receptor antagonists (Icatibant).
Context
Pathogenesis: Increased vascular permeability leading to extravascular fluid leak into subcutaneous sand submucosal tissues most notably face, lips, mouth, uvula, larynx, throat, genitalia, and bowel wall.
Etiology:
- Histaminergic (mast cell related):
- Often associated with urticaria and pruritis. Classic IgE mediated: allergic reactions – but other causes exist.
- Non-histaminergic (bradykinin related):
- Often associated with pain and pressure rather than pruritis.
Four subtypes:
- Decreased degradation:
- Angiotensin-converting enzyme inhibitors (ACEi) up to 32% of presentations (1). Typically within weeks of starting but can be years later.
- Dipeptidyl peptidase 4 inhibitors (DPP-4i) (gliptins): alogliptin, saxagliptin, sitagliptin and linagliptin.
∗∗ACEi treatment can uncover C1 inhibitor deficiency: beware of multifactorial causes of angioedema (2)**
- C1 inhibitor deficiency (increased bradykinin production):
- Acquired – may be associated with an underlying lymphoma, or monoclonal gammopathy.
- Hereditary Angioedema (HAE).
- Non-C1 inhibitor related: Hereditary angioedema (HAE).
- Idiopathic/Other:
- Infections (esp. in children).
- Idiopathic nonhistaminergic angioedema.
- Other drugs:
- Calcium channel blockers.
- Fibrinolytic agents – tPa, TNK etc. – rare but recognized complication. Treat as allergic reaction (even epinephrine if indicated).
Clinical Features:
- Onset minutes to hours; resolution hours to days.
- Asymmetric, non-pitting swelling of face, lips, mouth, uvula, larynx, throat, genitalia and/or bowel wall. (See https://emergencycarebc.ca/clinical_resource/anaphylaxis-diagnosis-treatment/).
- Bowel wall angioedema: abdominal pain, N/V/D, and may be seen on CT or U/S.
- May present as a surgical abdomen.
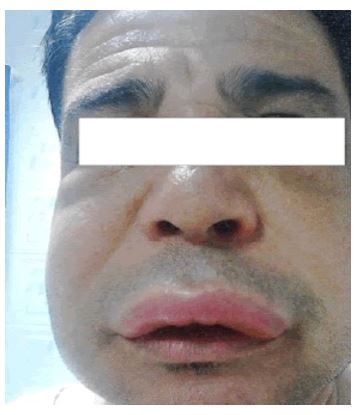

Images acquired from: Category:Angioedema – Wikimedia Commons [Internet]. commons.wikimedia.org. [cited 2023 Nov 29]. Available from: https://commons.wikimedia.org/wiki/Category:Angioedema
Diagnostic Process
Diagnosis is clinical.
History:
- Assess for rashes, locations of swelling.
- Recent insect bites/allergen exposures.
- Medication history: specifically, ACEi, DPP-4i, NSAIDs/Aspirin, estrogens, antibiotics,
- Any previous incidences of angioedema.
- FamHx of angioedema.
Physical Exam:
- Assess upper airway.
- Assess for anaphylactic shock.
- Assess for allergic symptoms – histaminergic features: urticaria (hives), itchy rash.
- Assess for lymphadenopathy as angioedema may be a first presentation of lymphoma (3).
Evaluation:
- If no mast-cell activation (allergic) related signs, the most likely etiology is bradykinin mediated.
Recommended laboratory testing: Limited value – may help with future work-up in community.
- Complement protein C4 and C1 inhibitor levels can be sent off for community follow-up if desired.
- With Urticaria: See clinical summary https://emergencycarebc.ca/clinical_resource/acute-urticaria/
Imaging: Abdo CT or US if indicated.
Recommended Treatment
- If a. signs of respiratory distress or b. hemodynamic instability, treat as anaphylaxis. See Anaphylaxis clinical summary.
- Get the help that you need EARLY, including ED staff (nurses, additional ERP), RT, and/or anesthesia/ENT if needed.
- Difficult airway identification: https://emergencycarebc.ca/clinical_resource/difficult-airway-identification-in-the-emergency-department/?_rt=NHwxfGludHViYXRpb258MTcwMTM2MzkzOQ&_rt_nonce=cfb63b3b0d
- Early intubation is recommended. Follow the appropriate clinical resource:
- Difficult airway management: https://emergencycarebc.ca/clinical_resource/difficult-airway-management/
- Rapid sequence intubation: https://emergencycarebc.ca/clinical_resource/rapid-sequence-intubation/
- When cause is unknown (often the case) treat for both allergic and non-allergic angioedema.
- Stop offending medications.
- Specific treatments:
- ACEi induced angioedema:
- Stop ACEi.
- Consider treatment with Tranexamic acid (TXA) 1g IV over 10 minutes (5).
- If severe, treatment with Icatibant 30mg SC q6h, max 90mg over 24 hours is indicated (a bradykinin B2 receptor antagonist).
- Treatment with 2 units of Fresh frozen plasma has shown some efficacy for the presence of ACE. which contains a C1 inhibitor, has been reported to be effective in acute attacks; however, there are rare reports of exacerbation of the angioedema by FFP.
- Anaphylaxis: See clinical summary. https://emergencycarebc.ca/clinical_resource/anaphylaxis-diagnosis-treatment/
- Allergic angioedema:
- H1 Antihistamines: eg. cetirizine up to 20 mg BID.
- Glucocorticoids: Prednisone in adults, prednisolone in children.
- Known or suspected hereditary angioedema: Treatment with a C1 inhibitor concentrate is indicated (icatibant most common) (4).
- BERINERT® (C1-Esterase Inhibitor) is a plasma-derived C1 Esterase Inhibitor (Human) indicated for the treatment of HAE attacks in adult and pediatric patients. Berinert is delivered intravenously and is approved for self-administration.
- FIRAZYR® (icatibant injection) is a bradykinin B2 receptor antagonist indicated for treatment of acute attacks of HAE in adults, adolescents and children aged 2 years and older with C1-esterase inhibitor deficiency. Firazyr is delivered by subcutaneous injection.
- A second line treatment is fresh frozen plasma, however this treatment has lower evidence and efficacy.
- Follow-up with hematologist/allergist.
- ACEi induced angioedema:
Underlying illness (e.g., Infection): treatment with antihistamines/glucocorticoids along with treatment of the illness, e.g., Antibiotics.
Criteria For Hospital Admission
- Respiratory distress, hemodynamic instability.
- Poor resolution or recurrence of symptoms if in areas of concern – airway or significant pain.
- Severe episodes can last for 3-5 days.
Criteria For Transfer To Another Facility
Dependent on resources available.
Criteria For Close Observation And/or Consult
- Impending respiratory failure.
- Hemodynamic instability.
- Resolved respiratory or hemodynamic instability – with/without treatment.
Criteria For Safe Discharge Home
- Patients should be monitored until symptoms are clearly resolving.
- Patients with allergic or anaphylactic angioedema have been provided education and requisition for EpiPen.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
This is a well described and documented topic, the majority of evidence is derived from high quality studies.
Related Information
OTHER RELEVANT INFORMATION
Hereditary Angioedema (HAE) Canada: https://haecanada.org/
Reference List
Gandhi J, Jones R, Teubner D, Gabb G. Multicentre audit of ACE-inhibitor associated angioedema (MAAAA). Aust Fam Physician. 2015;44(8):579–83.
Ricketti AJ, Cleri DJ, Ramos-Bonner LS, Vernaleo JR. Hereditary angioedema presenting in late middle age after angiotensin-converting enzyme inhibitor treatment. Ann Allergy Asthma Immunol [Internet]. 2007;98(4):397–401. Available from: http://dx.doi.org/10.1016/S1081-1206(10)60889-7
Gunatilake SSC, Wimalaratna H. Angioedema as the first presentation of B-cell non-Hodgkin lymphoma – an unusual case with normal C1 esterase inhibitor level: a case report. BMC Res Notes [Internet]. 2014;7(1). Available from: http://dx.doi.org/10.1186/1756-0500-7-495
Zuraw BL. Hereditary angioedema. N Engl J Med [Internet]. 2008;359(10):1027–36. Available from: http://dx.doi.org/10.1056/nejmcp0803977
Stoldt J, Cox C, Matusz E. Tranexamic acid use in the setting of ACE inhibitor induced angioedema. Am J Emerg Med [Internet]. 2022;55:230.e3-230.e4. Available from: http://dx.doi.org/10.1016/j.ajem.2022.01.041
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 15, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.