Bursitis – Diagnosis & Treatment
Orthopedic
Context
- Bursitis is inflammation or irritation of the bursa (a fluid-filled sac between layers of tissue to decrease friction and facilitate movement).
- Caused by infection (septic bursitis), direct trauma, overuse/prolonged pressure, or systemic illness like gout, ankylosing spondylitis, and rheumatoid or psoriatic arthritis.
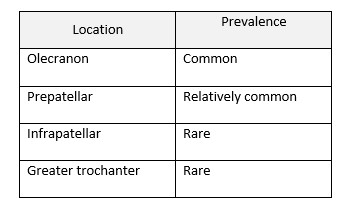
- Over 140 bursae in the body, however examples of some sites of bursitis include the following:
Diagnostic Process
Focused History and Physical Examination
- Pain (especially with movement), bursal enlargement, and tenderness.
- Need to differentiate between septic and noninfectious acute bursitis.
- Noninfectious bursitis: Warmth and erythema are less prominent, and the skin is intact.
- Septic bursitis: more abrupt onset with rapid progression over hours. The bursa is hot and erythematous, breaks in the overlying skin, +/- fever.
- Radiographic studies and ultrasound imaging not required unless concern for fracture.
- If considering infection, aspirate the bursa fluid: Gram stain, culture, cell count and crystals.
- Aspiration is both diagnostic and therapeutic.
Further lab work rarely indicated unless septic, want to rule in/out systemic illness.
Pitfalls
- Failure to recognize that a patient with less obvious bursitis: deeper and more chronic forms of bursitis can have no erythema or visible swelling.
- Failure to consider systemic conditions.
- Failure to aspirate the bursa when infectious process is a consideration.
- Failure to consider underlying septic joint.
Recommended Treatment
- Bursitis is usually self-limited, therefore the goals of treatment include symptom management, preventing disability and treating any underlying etiology if present.
- Superficial infectious bursitis = antibiotics for skin & soft tissue infection and drained via aspiration (some choose initial incision or drainage rather than aspiration).
- Arthrocentesis of the affected joint should be undertaken if signs of septic arthritis. (ex. Iliopsoas bursitis).
- Inflammatory bursitis should be treated with ice, rest, NSAIDs.
- Avoid further irritation or trauma to the bursa.
- Not typical ED treatment options:
- Corticosteroid injections have been shown to have similar long-term outcomes to physical therapy and lack high quality evidence demonstrating any acute benefits.
- Platelet-rich plasma injection (PRP) lacks high-quality evidence supporting its use and is therefore not recommended as part of the standard of care for bursitis.
- If there is an underlying systemic condition, treating the condition while advising conservative management is advised.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
There are currently no clinical trials or randomized control studies that recommend an evidence-based guideline for the management of bursitis.
Related Information
Reference List
Related Information
OTHER RELEVANT INFORMATION
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 05, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.