Cat and Dog Bites
Cardinal Presentations / Presenting Problems, Environmental Injuries / Exposures, Infections
First 5 Minutes
- Patients with extensive trauma and/or arterial injury should be placed in a trauma bay with an appropriate trauma approach.
- If the injury is isolated and non-arterial, an ambulatory zone is usually adequate.
- If arterial injury is suspected, consult vascular surgery.
Context
- The most prevalent mammalian bites in North America are from cats and dogs.
- Cats create deep puncture wounds that increase the risk of bacterial trapping and infection.
- Dogs often bite and shake their victim causing a “hole and tear” injury.
- Treatment recommendations are mostly based on historical dogma. Controversy remains on primary closure.
- Cat and dog bite wound infections are mostly polymicrobial. The most common bacteria include:
- Pasteurella multocida
- Capnocytophaga canimorsus
- Fusobacterium
- Bacteroides
- Porphyromonas
- Prevotella
- Propionibacterium
- Streptococci
- Staphylococci
- Moraxella
- Dog bite wound infections can also involve:
- Neisseria
- Corynebacterium
- C. animorsus acts as an encapsulated organism and can cause sepsis and DIC in immunocompromised patients, especially those with asplenia.
- The rate of wound infection from cat and dog bite are 10% to 40% and 6 to 16%, respectively. Infections include cellulitis, abscess, tenosynovitis, osteomyelitis (up to weeks later) and septic arthritis.
- Prophylactic antibiotics are not recommended universally, but all cat bites should be treated with antibiotics to cover Pasteurella.
- Risk factors for infection:
- Wound
- Devitalized tissue
- Primary closure may increase rate of infection
- Patient
- Age over 50
- Comorbid conditions resulting in immunocompromised status (e.g., cancer, diabetes, alcohol use disorder, etc.)
- Asplenia
- Wound
Diagnostic Process
- Key historical elements include the patient’s tetanus status and whether the animal has had a rabies vaccination (in BC, rabies has only been reported in bats, although cats or dogs can acquire rabies from bat exposures.) See https://emergencycarebc.ca/clinical_resource/rabies-diagnosis-and-treatment/
- A focused physical exam, including an assessment for infection or trauma.
- Obtain XRs if there is a concern for fracture, joint injury, or retained foreign body (e.g., teeth.)
- Consider CT head in a young child with a scalp bite to evaluate for intracranial penetration.
- Blood work and wound cultures are generally not indicated.
Recommended Treatment
Analgesia
Irrigation and debridement
- All bites require copious irrigation under pressure and debridement under local anesthesia. The only exemption is superficial cat bites, but not dog bites.
Wound closure
- Primary closure is controversial. The benefits (e.g., cosmesis) must be weighed against the risk of infection. Incorporate shared decision-making as appropriate. If closure is contraindicated, loose approximation using adhesive strips can improve cosmesis.
- There is general consensus for closure of scalp bites from any mammal if less than 6 hours old.
- Closure is NOT recommended in:
- All puncture or crush injuries.
- Delayed presentation over 6-8 hours.
- All wounds more than 24 hours old.
- Bite wounds over hands, feet, and joints.
- Cat or human bites (except on scalp.)
- Bite wounds in immunocompromised patients.
Antibiotics
- Cat bites:
- Antibiotic prophylaxis is indicated for ALL cat bites penetrating through the epidermis, regardless of location.
- Dog bites:
- Antibiotic prophylaxis is NOT indicated in all dog bites.
- Antibiotics are indicated for:
- Bites to the hand or foot.
- Deep puncture wounds.
- Bites in or near a prosthetic joint.
- Bites with significant tissue damage.
Antibiotics for cat and dog bites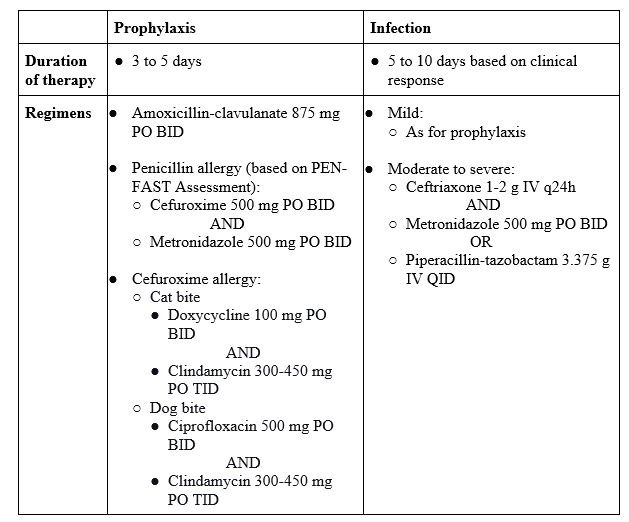
Immunization
- Tetanus prophylaxis +/- tetanus immunoglobulin, if indicated.
- Rabies prophylaxis, if indicated.
Criteria For Hospital Admission
- Injuries requiring reconstructive surgery and/or general anesthesia.
- Rapidly spreading skin and soft tissue infections.
- Bacteremia or sepsis.
- Osteomyelitis, septic arthritis, infectious tenosynovitis.
- Failed outpatient therapy.
Criteria For Transfer To Another Facility
- In exceptional cases of worsening patient status that cannot be managed by resources at the current care facility, transfer to another facility is warranted.
Criteria For Safe Discharge Home
- Patients with uncomplicated bites can safely be discharged home with return precautions.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Antibiotic prophylaxis:
- Strong evidence to support antibiotic prophylaxis for cat bites (penetrating past the epidermis) and dog bites to the hands.
- Mixed data to suggest the use of antibiotic prophylaxis for all dog bites. The current recommendation is to limit prophylaxis in dog bites to high-risk wounds only.
Primary closure: Studies report no significant differences in the rates of infection between primary closed dog bites and wounds left open. Clinical judgement required.
Related Information
Reference List
Maniscalco K, Edens MA. Animal Bites. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 Jul 8]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK430852/
Kheiran A, Palial V, Rollett R, Wildin CJ, Chatterji U, Singh HP. Cat bite: an injury not to underestimate. J Plast Surg Hand Surg. 2019 Dec;53(6):341–6.
Kennedy SA, Stoll LE, Lauder AS. Human and other mammalian bite injuries of the hand: evaluation and management. J Am Acad Orthop Surg. 2015 Jan;23(1):47–57.
Wound Management Principles – ClinicalKey [Internet]. [cited 2023 Jul 8]. Available from: https://www.clinicalkey.com/#!/content/book/3-s2.0-B9780323757898000505?scrollTo=%23hl0000617

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 21, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.