Chest Pain: Ruling Out Acute Coronary Syndrome
Cardinal Presentations / Presenting Problems, Cardiovascular
Context
- Chest pain is one of the most common presentations to the emergency department (ED) and approximately 10 – 15% of such patients will have an acute coronary syndrome. (ACS; either acute myocardial infarction or unstable angina).
- This approach applies to:
- stable patients
- suspected ACS only and cannot be used to rule out other causes such as pulmonary embolus or aortic dissection
- patients with no other clear cause for their pain.
- Stable patients have the following features: normal vital signs, no evidence of ischemia on EKG, (no ST elevations or depressions, and no T wave inversions) no ongoing pain in the ED, and negative troponin(s).
- Stable patients do not require cardiac monitoring while awaiting serial troponins.
- 20-30% of these patients do not need further testing. We can determine who can go home within 2-3 hours and who can go home after within 6 hours. The result is increased patient satisfaction, decreased ED crowding, and a reduction in unnecessary testing.
The Diagnostic Process
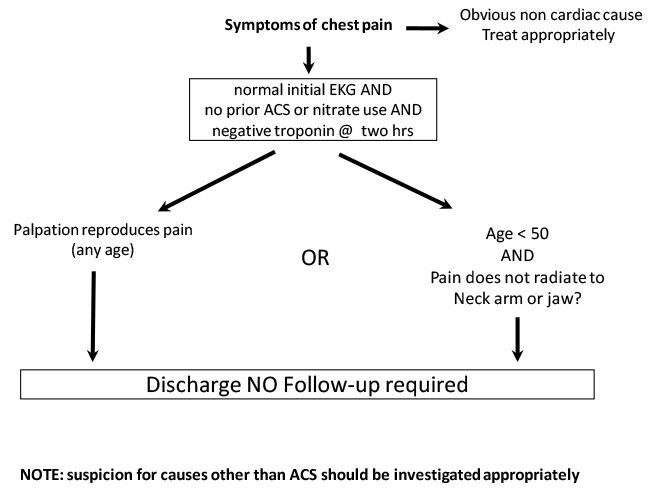
- Patients who are under 50 with no prior ACS or nitrate use, and who have normal EKGs and troponin at 2 hours, can be safely discharged home with no follow-up testing.
- Patients over 50 with no prior ACS or nitrate use, a normal EKG and negative troponin at 2 hours AND who have pain reproducible with direct palpation, can also be safely discharged home with no follow-up testing.
- Patients with an elevated troponin or abnormal EKG and no other cause for their pain should be referred for further investigation.
- Patients who do not fall into the above categories should undergo ED observation with sequential investigations (EKGs and troponins) over 6 hours. If all investigations are normal, they should have outpatient follow-up with a cardiologist or internist within two weeks. Ideally, the emergency physician can arrange ancillary outpatient investigations within 48 hours to be followed by a cardiologist or internist in a similar time frame.
- Patients should be encouraged to take ASA and return if their pain recurs.
Vancouver Chest Pain Rule
Outpatient Investigations
- Exercise stress tests (EST) are functional investigations that have ~70% sensitivity and specificity for ACS. Patients must have normal resting EKGs and be able to walk for 12 minutes.
- Myocardial perfusion scanning is a functional test with similar sensitivity and specificity as EST for ACS. However, patients with diffuse disease may be false-negatives.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
There are validated studies for both the 2 – hour and 6 – hour decision aids. Although the specifics are slightly different, this approach is similar to those in other settings. (see Than M, et al. Lancet. 2011; 377: 1077 – 1084)
The 0/1-h early rule-out algorithm for ACS using high-sensitivity troponin has been prospectively validated with a NPV of 99.9% (see Twerenbold R, et al. Am Coll Cardiol 2017)
Related Information
OTHER RELEVANT INFORMATION
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Cardiovascular EmergenciesRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Sep 15, 2018
Visit our website at https://emergencycarebc.ca
COMMENTS (8)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.