Clavicle Fracture – Diagnosis and Treatment
Orthopedic, Trauma
Context
- Accounts for approximately 2.6% of all fractures1 with peak incidence occurring in children and young adults. The clavicle is the most fractured bones in children4.
- The clavicle is the only osseous link between the upper extremity and chest wall. It is thin, superficial, and prone to fracture during a fall.
- 2 coracoclavicular (CC) ligaments at the distal end stabilize superior and inferior movement. Disruption of these ligaments in the context of a fracture is unstable and has a high incidence of non-union.
- Critical structures that are vulnerable to damage by clavicular fragments include the subclavian artery/vein, the brachial plexus, and the lung apex.
Diagnostic Process
History and Physical
- Most commonly occurs from a fall/impact to the shoulder4. Less commonly from falling on an outstretched hand or direct blow to clavicle.
- The head may be tilted to the affected side and the affected arm may be held low and close to the body.
- Common findings include focal tenderness, ecchymosis, swelling, crepitus, and visible/palpable deformity.
- Ensure there is no open fracture or skin tenting, perform a neurovascular exam, and consider associated injuries such as pneumothorax or other fractures.
Imaging
- Obtain upright views to avoid underestimation of displacement.
- Standard clavicle views include an AP clavicle as well as 15o cephalic tilt view.
- CXR can be considered for ruling out pneumothorax.
- Consider CT if there is significant proximal clavicular displacement as any potential intrathoracic damage should be further delineated.
Diagnostic considerations
- Always assess the neurovascular status of the affected limb, as the subclavian artery/vein and brachial plexus are located anatomically close.
- Consider CT to further evaluate when concerned for vascular injury.
- Consider pneumothorax/hemothorax, especially if the proximal clavicle is involved.
- Proximal clavicle fractures are typically associated (90%) with major trauma/injury and require a thorough examination2. They are uncommonly isolated injuries.
- Concomitant ipsilateral scapular neck fractures leave the shoulder disconnected from the chest wall. These injuries are called “floating shoulders” and require orthopedic referral.
Recommended Treatment
Indications for Orthopedic Referral
- Significant practice pattern variation may exist between institutions. Absolute indications for orthopedic referral include open fractures/skin tenting, neurovascular compromise, floating shoulder and severe displacement/comminution/shortening.
- Proximal 3rd fractures with any clinically significant displacement warrant referral due to proximity to critical intrathoracic structures.
- Distal 3rd fractures with CC ligament disruption warrant referral as these are unstable fractures.
- Consider referral for high level athletes, cosmetic concern, or significant seizure/neuromuscular disorder.
Non-operative management
- Immobilization is the mainstay of treatment, continue until clinical union is achieved (non-tender and full painless ROM).
- A sling for comfort is suggested.
- A figure of 8 bandage is no longer recommended due to similar outcomes, more pain and risk of complications3.
- Early elbow range of motion exercise is encouraged throughout immobilization.
Disposition
- Majority heal uneventfully.
- Fractures which do not require surgical referral can be seen by primary care physicians in 1-2 weeks.
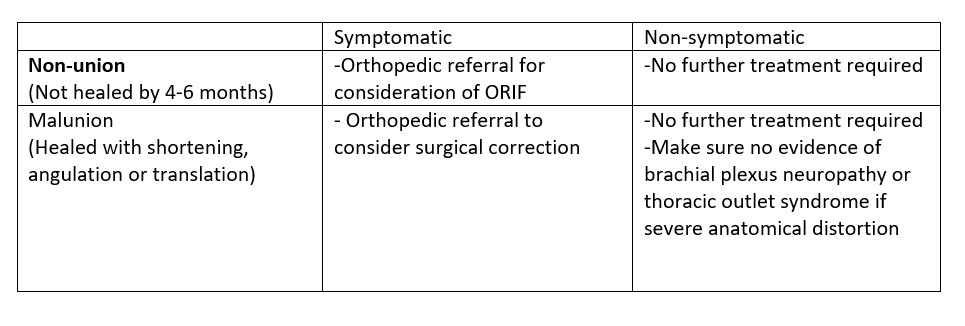
Complications
Pediatric Considerations
- Non-operative treatment is usually effective, leading to faster clinical union than in adults (3-4 weeks).
- Any clavicular bowing (no cortex disruption) should be treated as a fracture.
- Unlike adults, distal fractures involving CC ligament disruption are not always unstable due to the periosteal sleeve often remaining intact, preventing displacement. Conservative management is appropriate in the absence of displacement.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Significant variation in practice exists and the nuances of definitive treatment remain controversial.
Related Information
Reference List
Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002; 11:452-456
Throckmorton T, Kuhn JE. Fractures of the medial end of the clavicle. J Shoulder Elbow Surg 2007; 16:49.
Ersen A, Atalar AC, Birisik F, et al. Comparison of simple arm sling and figure of eight clavicular bandage for midshaft clavicular fractures: a randomised controlled study. Bone Joint J 2015; 97-B:1562.
Walls RM, Hockberger RS, Gausche-Hill M, Erickson TB, Wilcox SR. Shoulder Injuries. In: Rosen’s emergency medicine: Concepts and clinical practice. 10th ed. Philadelphia, PA: Elsevier; 2023.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 08, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.