Congenital Heart Disease (Adult Survivors)
Cardiovascular
Context
- Due to improvements in pediatric surgery techniques, the number of Congenital Heart Disease (CHD) adult survivors has increased.
- Over a 5 year period, a study in Canada found that 50% of adult congenital heart disease survivors were hospitalized and 68% used the emergency department.
- The most common way congenital heart disease adult survivors present to the ER is in an arrhythmia, which is responsible for 37% of hospital admissions.
- 1/5 adults with CHD have used the ER.
Diagnostic Process
Palpitations/syncope
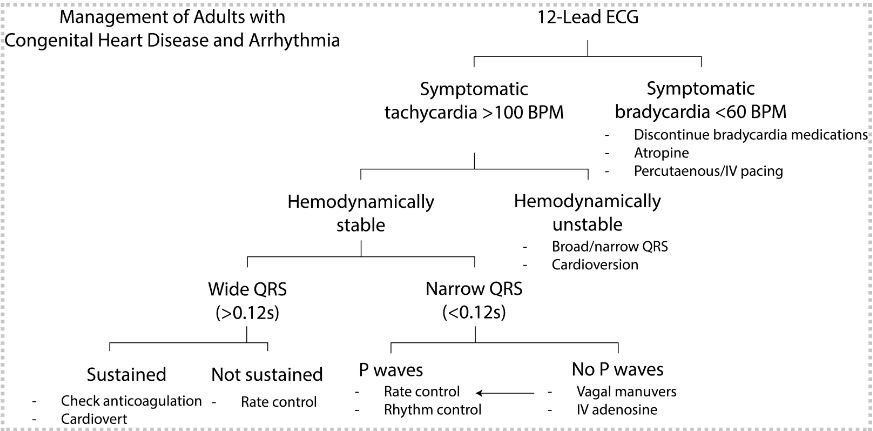
- A 12-lead ECG should be completed.
- Atrial tachycardia is the most commonly detected arrythmia in patients with CHD and can result in syncope or sudden cardiac death if there is 1:1 conduction through the AV node.
- Patients with surgically corrected tetralogy of Fallot have a higher incidence of Ventricular Tachycardia.
- Increased incidence of atrioventricular block in those with atrioventricular septal defects or surgically corrected transposition of the great arteries.
SOBOE, pitting edema, paroxysmal nocturnal dyspnea, orthopnea
- Symptoms suggestive of heart failure.
- ECG, CXR, CBC, lytes, Cr, BNP +/- troponin.
- Ask about any recent surgeries because of the possibility of surgical complications including infection, pericardial effusion and pacemaker displacement.
Cyanotic heart disease is an umbrella term for disorders caused by right to left shunting of blood. Physical exam findings for those with cyanotic heart disease include bluish discolouration of skin and mucous membranes, dependent on the extent of compensatory erythropoiesis.
Created by Ella Chan, UBC MSI 2023
Recommended Treatment
These are structurally complex patients from a cardiovascular standpoint. Treatment would, in general, be done with your cardiology consultant.
Arrhythmias
- Atrial tachycardia
- If hemodynamically unstable, cardioversion is needed immediately irrespective of coagulation status, with electrical cardioversion being the recommended option.
- If hemodynamically stable, patient could undergo pharmacological treatment or follow-up with a cardiologist for consideration of an invasive approach to management. The decision to leave the patient in atrial tachycardia requires consultation with a specialist and is contingent upon adequate rate control, and could allow for more accurate identification of the substrate/erroneous circuitry for ablation.
- Ventricular arrhythmias
- Electrical cardioversion used to terminate VT.
Bradyarrhythmia
- Atropine and percutaneous pacing (short-term solution) are to be used in emergencies, while cardiology/internal medicine is consulted for transvenous pacing options.
Heart Failure
- Increased bleeding and thrombosis risk in acute HF presentations in CHD patients. According to European guidelines, coagulation platelets and clotting factors should be assessed and phlebotomy may be considered if hematocrit > 65%.
- No trials specific to managing Heart Failure in CHD patients but the guidelines pertaining to the general population can be applied on a case-by-case basis.
Long-term Complications of Cyanotic Heart Disease
- Secondary erythropoiesis and microcytosis (due to inadequate iron stores) leading to hyper viscosity and increased cerebrovascular risk. Phlebotomy is occasionally done in consultation with an expert.
- In patients with right-to-left shunt, risk of paradoxical emboli and stroke, so threshold to do head imaging should be lower. If patient needs intravenous lines, an air filter can reduce risk of air emboli.
- Hemoptysis secondary to pulmonary HTN where a CT Pulmonary Angiogram should be done emergently.
- Increased risk of thromboembolism but routine anticoagulation or antiplatelet agents are not recommended.
- Increased erythropoiesis results in increased unconjugated bilirubin production, thereby increasing risk of pigment gallstones. Surgery is not advised in patients who are asymptomatic.
- 2015 American Heart Association guidelines recommend that patients with unrepaired cyanotic heart disease undergo exercise testing before partaking in sports and exercise.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Very few studies done studying adult survivors of congenital heart disease and their presentation to the emergency department. There are currently no international guidelines on this topic. Moreover, there are no trials specific to managing Heart Failure in CHD patients and the Canadian Cardiovascular Society Consensus on CHD does not comment on managing Heart Failure or arrhythmias in this unique population.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Budts, W., Roos-Hesselink, J., Rädle-Hurst, T., Eicken, A., McDonagh, T., Lambrinou, E., Crespo-Leiro, M., Walker, F. and Frogoudaki, A., 2016. Treatment of heart failure in adult congenital heart disease: a position paper of the Working Group of Grown-Up Congenital Heart Disease and the Heart Failure Association of the European Society of Cardiology. European Heart Journal, 37(18), pp.1419-1427.
Chessa, M., Brida, M., Gatzoulis, M., Diller, G., Roos-Hesselink, J., Dimopoulos, K., Behringer, W., Möckel, M., Giamberti, A., Galletti, L., Price, S., Baumgartner, H., Gallego, P. and Tutarel, O., 2021. Emergency department management of patients with adult congenital heart disease: a consensus paper from the ESC Working Group on Adult Congenital Heart Disease, the European Society for Emergency Medicine (EUSEM), the European Association for Cardio-Thoracic Surgery (EACTS), and the Association for Acute Cardiovascular Care (ACVC). European Heart Journal, 42(26), pp.2527-2535.
Connolly, H., 2020. Medical management of cyanotic congenital heart disease in adults. [online] UpToDate. Available at: <https://www.uptodate.com/contents/medical-management-of-cyanotic-congenital-heart-disease-in-adults?search=congenital%20heart%20disease&source=search_result&selectedTitle=5~150&usage_type=default&display_rank=5#H682401768> [Accessed 7 January 2022].
De Backer, J. and Budts, W., 2019. What a general cardiologist should know about adult congenital heart disease. [online] European Society of Cardiology. Available at: <https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-18/what-a-general-cardiologist-should-know-about-adult-congenital-heart-disease> [Accessed 7 January 2022].
-
Mital, S., Therrien, J. and Silversides, C., 2010. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: Introduction. Canadian Journal of Cardiology, 26(3), pp.e65-e69.
Silversides, C., Marelli, A., Beauchesne, L., Dore, A., Kiess, M., Salehian, O., Bradley, T., Colman, J., Connelly, M., Harris, L., Khairy, P., Mital, S., Niwa, K., Oechslin, E., Poirier, N., Schwerzmann, M., Taylor, D., Vonder Muhll, I., Baumgartner, H., Benson, L., Celermajer, D., Greutmann, M., Horlick, E., Landzberg, M., Meijboom, F., Mulder, B., Warnes, C., Webb, G. and Therrien, J., 2010. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: Executive summary. Canadian Journal of Cardiology, 26(3), pp.143-150.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 07, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.