Depression
Psychiatric and Behaviour
First 5 Minutes
- A structured risk assessment should be conducted including risk of self-harm, suicide or risk of harm to others.
- No tool is 100 percent accurate.
Context
Emergency Department visits for mental health have increased by 20% over the past decade.
Factors contributing to ED visits for mental health reasons include:
- Age 12 to 24 years
- Immigrants
- Low socioeconomic status
- Identifying as gender non-binary
- Co-occurring substance use disorders
- Experiencing homelessness or marginal housing
- Elderly (may be misdiagnosed as early dementia)
Long-term consequences of depression include increased mortality and morbidity rates.
Diagnostic Process
Various presentations:
- Non-specific somatic complaints such as headache, chronic pain, weakness, fatigue.
- Suicidal ideation or attempt.
- Under the influence of substances.
The PHQ-2 screening tool can be used to assess key symptoms related to depression. It has comparable specificity and sensitivity to the PHQ-9.
Two questions can be asked: “Over the last 2 weeks, how often have you been bothered by any of the following problems”
- Little interest or pleasure in doing things (Anhedonia).
- Feeling down, depressed or hopeless.
Each PHQ-2 question is scored from 0 to 3
- Not at all = 0
- Several days = 1
- More than half the days = 2
- Nearly every day = 3
If score of 3 or higher, the patient requires a thorough assessment or PHQ-9.
Recommended Treatment
Communication tips for interacting with depressed patients in the ED:
- Establish rapport.
- Respond with empathy.
- Avoid leading questions and utilize open-ended questions.
- Assess whether a patient requires further consultation from a psychiatrist.
- Obtain collateral information to assist in evaluation.
- Ask screening questions for suicidality.
SAD PERSONS is one approach to assess suicide risk. No tool accurately determines suicide risk.
S – Male Sex = 1 point
A – Age < 19 or > 45 years = 1 point
D – Depression = 2 points
P – Previous Attempt = 2 points
E – Excess alcohol or substance use = 1 point
R – Rational thinking loss = 2 points
S – Social supports lacking = 1 point
O – Organized plan = 2 points
N – No spouse = 1 point
S – Sickness = 1 point
- It allots a point of one for: male sex, age < 19 or > 45, previous attempts / psychiatric care, excessive alcohol / drug use, individuals that are separated / divorces / widowed and lack of social supports.
- It allots two points for: depression / hopelessness, loss of rational thinking, attempts (serious or organized) and stated future intent.
- Based on an individual’s total score they are risk stratified as follows:
- 0-2 = send home with follow-up
- 3-4 = close follow-up, consider hospitalization
- 5-6 = strongly consider hospitalization
- 7-10 = hospitalize
1st line medication recommendations for depression SSRIs and SNRIs (dosage varies depending on specific medication) but may include:
- Agomelatine (Valdoxan 25-50mg)
- Bupropion (Wellbutrin 150-300mg)
- Mirtazapine (Remeron 15-45mg)
Relative differences between first line medications are small and there are no absolutes when choosing one to prescribe over the other.
Consider providing resources for counselling, especially for isolated patients or those with a lack of social supports (e.g., family, friends)
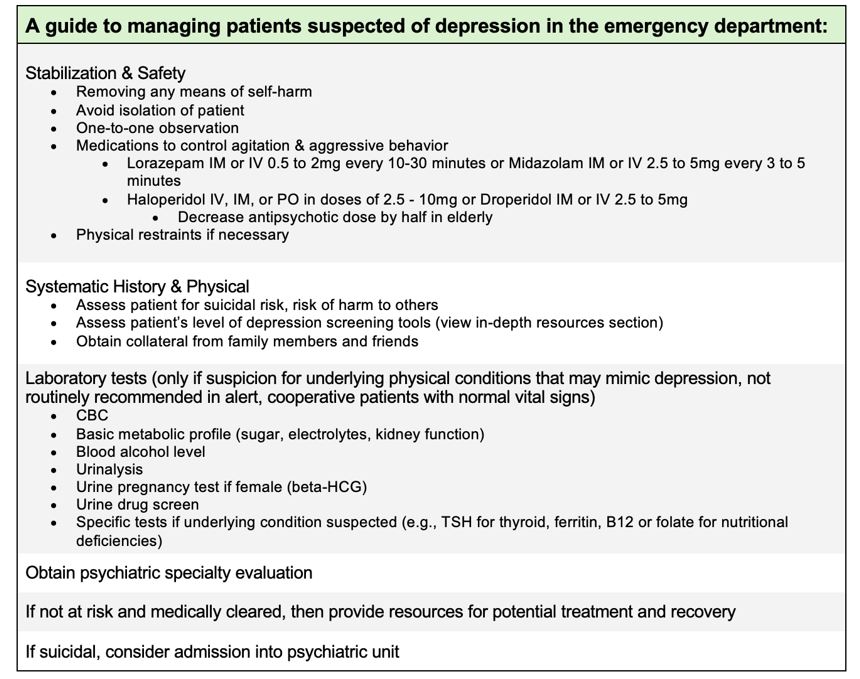
Table 1. Emergency department management of patients with depression.
Criteria For Hospital Admission
- Admit if the patient poses a risk of harm to themselves or others.
- Also consider admission in patients with severe symptoms of depression, even if without active suicidal ideation, potentially on an involuntary basis.
Criteria For Safe Discharge Home
- Patients may be discharged when they are deemed to pose a low risk of harm to themselves or others.
- Patients should receive instructions and resources on managing their medications, activities of daily living and follow-up with appropriate services (e.g., Psychiatric or GP follow-up, housing, financial needs).
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Depression management guidelines in the Emergency Department.
Diagnosis and screening of depressive disorders.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Shyman L, Sukhorukov R, Barbic D, Mathias S, Chau S, Leon A, et al. Social Determinants of health and depression in adults presenting to the Emergency Department. Canadian Family Physician. 2021 Dec;67(12). doi:10.46747/cfp.6712e337
Kuo DC, Tran M, Shah AA, Matorin A. Depression and the suicidal patient. Emergency Medicine Clinics of North America. 2015 Nov;33(4):765–78. doi:10.1016/j.emc.2015.07.005
Moore GP, Moore MJ. Assessment and emergency management of the acutely agitated or violent adult [Internet]. 2023 [cited 2024 Jan 27]. Available from: https://www.uptodate.com/contents/assessment-and-emergency-management-of-the-acutely-agitated-or-violent-adult
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 21, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.