Endocarditis Diagnosis and Treatment
Infections
Context
Endocarditis is an inflammation of the endocardium, with an in-hospital mortality rate of 14-22%
- Often present with fever of unknown origin
- Vegetations on the cardiac valves are the hallmark: bacterial or fungal in infective endocarditis (IE) or sterile (non-infective endocarditis)
- IE is uncommon, with an incidence of 3 to 7 per 100,000 person-years; IE is more common than non-IE.
Risk factors for IE include:
-
-
- Prior damage to heart valves i.e. rheumatic heart disease, congenital heart disease, prosthetic valves, or prior endocarditis.
-
Intravenous drug use, poor dentition, indwelling catheters, chronic hemodialysis, invasive procedures, or other potential causes of bacteremia.
-
-
- Age >60.
- Complications: embolic phenomena, valvular insufficiency, heart failure, and distant infection.
- 90% of IE is left-sided, affecting the mitral valve or aortic valve:
- Left-sided IE is associated with systemic emboli.
-
In intravenous drug users 76% of IE is right-sided, predominantly affecting the tricuspid valve:
-
-
- Right-sided IE is associated with pulmonary emboli rather than systemic findings.
- Patients with suspected IE should be admitted to the hospital, with specialist consultation and initiation of antibiotic therapy.
-
Diagnostic Process
Infective endocarditis:
- The majority present with fever. Other symptoms and signs of IE include constitutional symptoms, headache, myalgias, arthralgias and new cardiac murmurs.
Signs of IE include:
- Vascular emboli: Janeway lesions, splinter hemorrhages and conjunctival hemorrhage.
- Immune complex phenomena: Osler’s Nodes (painful erythematous nodules on fingers) and Roth’s spots (retinal hemorrhages).
- Critical diagnostic tests are blood cultures and echocardiography.
- Prior to antibiotic treatment, three sets of blood cultures must be drawn from different venipuncture sites, with the first and final cultures being drawn at least one hour apart. Note that 5-10% of IE cases are blood culture-negative (due to infection by a non-culturable pathogen, antimicrobial treatment prior to culture collection, or poor microbiological technique).
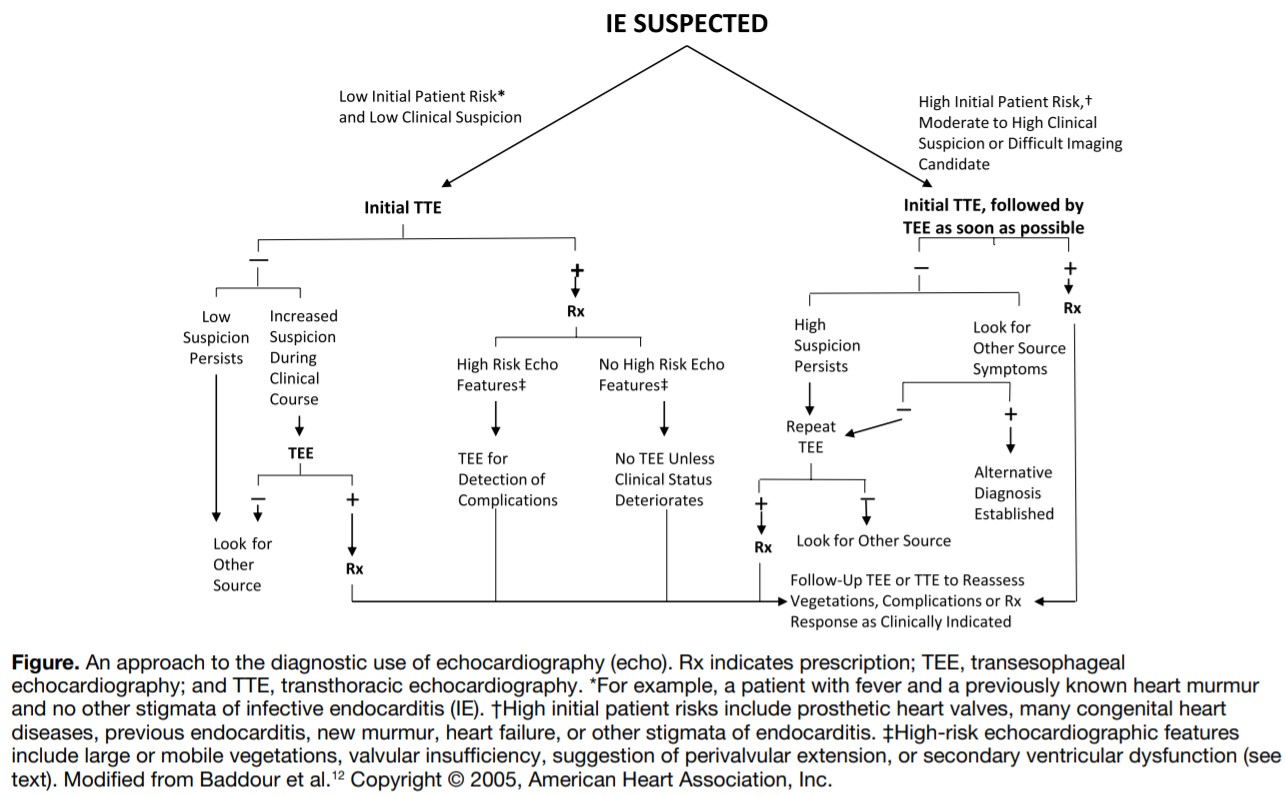
- Urgent echocardiography should be completed (within 12 hours of presentation). Transthoracic echocardiography (TTE) is often the initial imaging modality, though it is less sensitive than transesophageal echocardiography (TEE). TEE should follow TTE as quickly as possible in highly suspected cases of IE.
- A minority of IE patients present with the classic Oslerian manifestation: bacteremia/fungemia, valvular vegetations, peripheral emboli and immunological phenomena
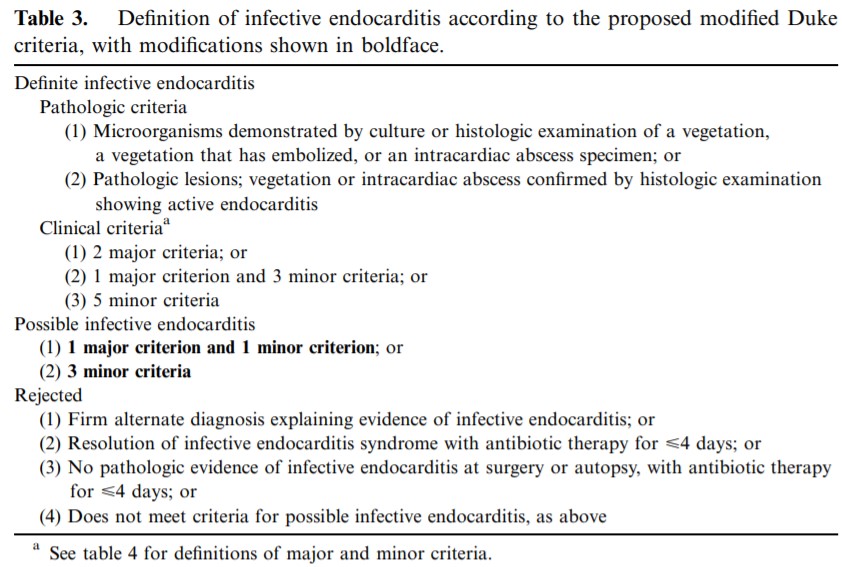
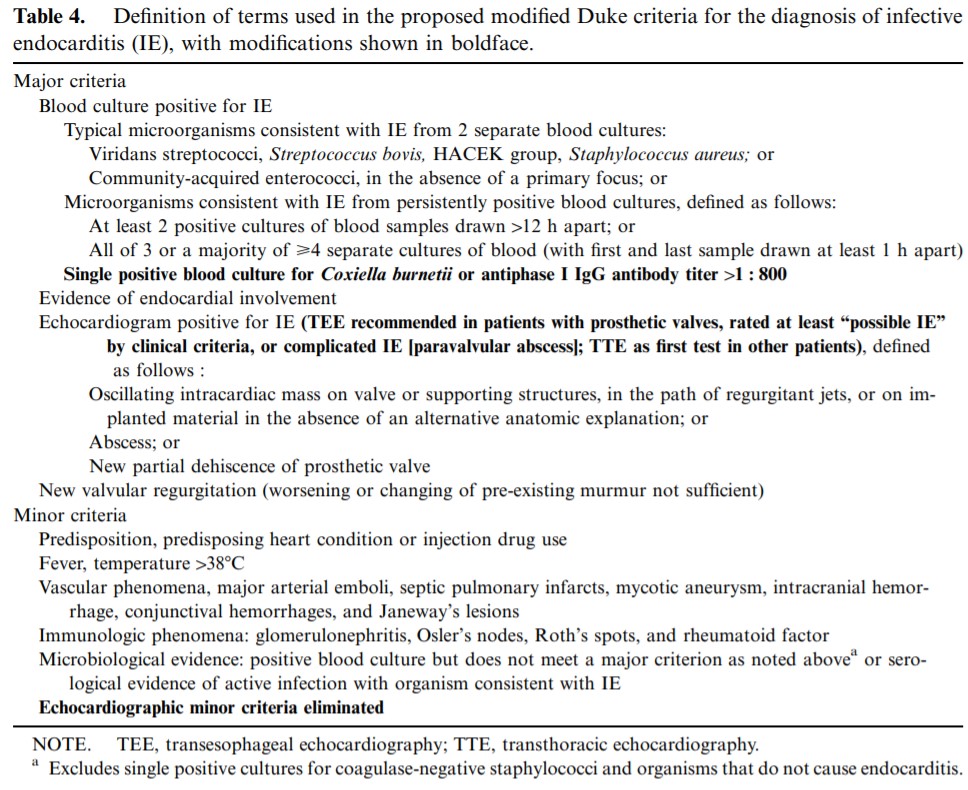
- Diagnosis is aided using the Modified Duke Criteria (published by Li et al. in 2000), which describe the criteria for diagnosis of Definitive IE, Possible IE, or Rejection of IE:
Recommended Treatment
- The most common etiologies of infective endocarditis are gram-positive bacteria: Staphylococcus aureus, Viridans Group Streptococcus, and Enterococcus.
- Less common etiologies include fastidious gram-negative bacilli which are slow to culture: Haemophilius, Aggregatibacter, Cardiobacterium hominis, Eikenella corrodens and Kingella
- IE caused by Candida is rare but serious; survival is less than 20%
- For patients with native valve IE who do not use IV drugs, empiric antibiotic treatment is vancomycin (15mg/kg IV q8-12h) plus ceftriaxone (2g IV daily).
-
In IV drug users
- Empiric antibiotic treatment is vancomycin (15mg/kg IV q8-12h) plus one of gentamicin (1.5-2mg/kg IV q8h), tobramycin (1.5-2mg/kg IV q8h), or ciprofloxacin (400mg IV q12h or 750mg PO bid).
-
In patients with a prosthetic valve
- Empiric antibiotic treatment is vancomycin (15mg/kg IV q8-12h), gentamicin (1mg/kg IV q8h) and rifampin (300mg PO tid or 600mg PO bid), with or without fluconazole (800mg IV or PO daily). Ciprofloxacin (400mg IV q12h or 750mg PO bid) may be selected in place of gentamicin. Begin rifampin 3-5 days after vancomycin and gentamicin to reduce the incidence of resistance.
- Indwelling catheters and devices may need to be removed.
- Early surgical consult should be obtained in patients with heart failure, conduction block, abscess, difficult to treat pathogens, persistent infection, and large vegetations.
- Treatment is often multidisciplinary with consultation from cardiology, infectious disease, and cardiac surgery specialists.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
High; the modified Duke Criteria have been validated across multiple studies. Antibiotic recommendations are based on randomized controlled trials.
Related Information
Reference List
-
Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): The Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC) 30(19):2369-2413.
Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, Moreillon P, Antunes M, Thilen U, Lekakis J, Lengyel M, Muller L, Naber C, Nihoyannopoulos P, Moritz A, and Zamorano J.
–European Heart JournalManagement of infective endocarditis. 2006; 92:124-130.
Habib G.
-Heart | BMJ JournalsInfective Endocarditis. (2013; 368:1425-1433.)
Hoen B and Duval X.
–N Engl J Med-
-
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 01, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.