Falls in Geriatric Patients
Cardinal Presentations / Presenting Problems, Special Populations, Trauma
Context
- Older adults (65 years and older) make up 30% of BC Emergency Department visits.
- Falls are very common. 1/3 of older adults have at least one per year.
- They are more likely to present unwell and require admission.
- Challenging to diagnose due to difficulties in history taking, vague/delayed presentations, underlying comorbidities and polypharmacy.
- Physiological changes include impaired immune response, decreased cardiac functional reserve, decreased peripheral sensation and blood supply, impaired renal function, altered medication metabolism.
- Consider older adult as a “beta blocked immunocompromised 50-year-old”.
- Vitals are unreliable.
- Heart rate of 100 may represent maximal tachycardia (especially if calcium channel or beta blockers).
- Systolic blood pressure of 120 may represent hypotension if chronically hypertensive.
- Traditional “mechanical” fall management is focused on traumatic injury, but there is increased recognition that falls represent larger dysfunction and geriatric falls syndrome.
- Movement away from term ‘mechanical fall’. This inaccurately implies a benign source (i.e. external mechanical force causing fall).
- Consider term “non-syncopal” fall instead.
- Fall is likely a sign of underlying issue: postural hypotension, polypharmacy, loss of muscle tone or difficulty with gait, balance, vision or proprioception.
- High associated morbidity and mortality:
- 1/3 ED patients with minor falls will functionally decline within 3 months.
- Most patients can be discharged, but a high suspicion for underlying pathology and recognition of geriatric considerations needed.
Context
Recommended steps in ED management of falls.
Cause of Fall
- Conduct full history to differentiate from syncope (cause/location of fall, time on ground, loss of consciousness or altered mental status, melena, substance use, prior falls or gait/balance difficulties).
- If patient is confused, obtain collateral and determine baseline.
- Consider atypical presentations contributing to fall:
- Alcohol use common but under recognised.
- Elder abuse underreported and increasing, consider in head/neck/upper extremity injuries, delay to presentation, signs of neglect.
- Depression associated with falls. More likely to be somatic complaints (sleep, pain, anxiety) versus mood.
- Rule out medical cause: cardiac, infection, GI bleed, metabolic or electrolyte dysfunction, seizure, stroke, etc.
- Conduct full head to toe exam noting neuropathy or strength deficits, +/- orthostatic vitals.
- Obtain CBC, electrolytes, renal function, medications levels (e.g. digoxin), ECG.
- Troponin, serum toxicology screen (salicylates, acetaminophen, ethanol), extended electrolytes, blood cultures may be indicated.
Injuries
- Commonly lower extremity, trunk/spine and skull/intracranial.
- More likely to sustain skeletal injury (fragile bones), occult bleeding (fragile vessels, anticoagulation), intracranial injury (fragile brain, atrophy).
- Conduct full exam. Patient may lack awareness of physical issue (impaired sensation).
- Extremity, hip/pelvis, thoracic or lumbar X-rays if clinical concern.
- Lack of clinical decision rules for imaging head/cervical spine in older patients.
- Low threshold for imaging based on mechanism (exam may be unreliable).
- Generally, all older patients with head injury require CT head if anticoagulated.
- X-rays of cervical spine unreliable, CT higher yield.
Safe Discharge Plan
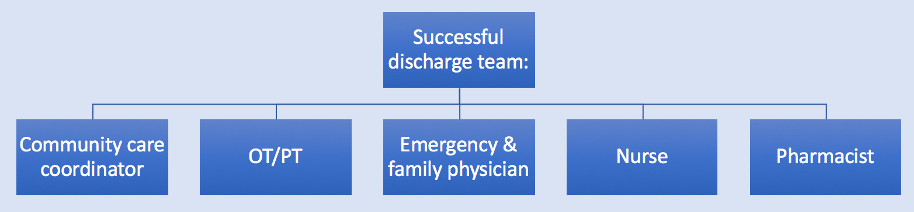
- Ideally multi-disciplinary team (in addition to family), depending on setting may include:
- Estimate future falls risk, considering risk factors:
- Prior falls (especially if associated injuries)
- Polypharmacy (especially benzodiazepines, anticholinergics, sedatives)
- Impaired hearing, eyesight or proprioception
- Loss of mobility
- If no PT, consider performing timed “up and go” test. The time to rise from chair and take 6 steps (3 metres), predicts increased falls risk if >15 seconds.
- De-prescribe inappropriate medications associated with fall, or at minimum flag for family physician follow-up.
- Minimize delirium development risk in ED by encouraging monitor removal, mobilizing, feeding, ordering home medications and oral analgesics as needed.
- Admission Criteria:
- Systemic illness
- Cardiac syncope (e.g. no symptoms prior to syncopal fall or new rhythm abnormality)
- Pathological (insufficiency) fracture
- Ongoing medication issue (e.g. supratherapeutic cardiovascular or hypoglycemic medication)
- Increasing falls without obvious cause
Prevent Future Falls
- Low grade evidence that moderate balance/mobility exercise may help reduce risk (e.g. Tai-chi).
- If you have access to falls or geriatrics clinic, refer high-risk patients.
- For low impact falls causing fracture, emphasize family physician follow-up for osteoporosis management.
- Emphasize to patient that fall is potentially lethal and encourage follow up appointment attendance.
Recommended Treatment
- Serial CT head to rule out delayed intracranial hemorrhage in anticoagulated patients after 24 hours generally not recommended in BC.
- Overall incidence low, consider associated cost, resource strain and radiation.
- Counsel about delayed bleed and return to ED.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Some conflicting evidence. Generally serial CT head not recommended. The vast majority of clinically relevant intracranial hemorrhage will be identified on initial imaging.
Related Information
OTHER RELEVANT INFORMATION
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 06, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.