Fibrinolytic Therapy for STEMI
Cardiovascular
Context
- Fibrinolytic therapy is recommended for the treatment of ST-elevation myocardial infarction (STEMI) and remains a suitable alternative reperfusion strategy for those unable to undergo timely primary percutaneous coronary intervention (PPCI).
- Administration of fibrinolytics is given a Class I recommendation for STEMI reperfusion if given within 12 hours of symptom onset and if angiography cannot be achieved in 2 hours or less.
- 64% of B.C. citizens age ≥ 40 years reside within 120 minutes of a PCI-capable centre. The national average is 80%.
- Fibrinolytic therapy has its greatest benefit the earlier it is administered; up to 30% of STEMIs can be successfully aborted if fibrinolytics are given within the first hour of symptom onset.
Recommendations and Dosing
- If PPCI is not accessible within 120 min of first medical contact (FMC), fibrinolysis should be considered. Quality processes should target a FMC-to-needle time ≤ 30 min. FMC can either be in the field with a first responder (e.g. paramedic) or after patient presentation to a hospital emergency department (ED).
- Among the available options, fibrin-specific fibrinolytics such as tenecteplase (TNK) or accelerated infusion alteplase (tPA) are preferred.
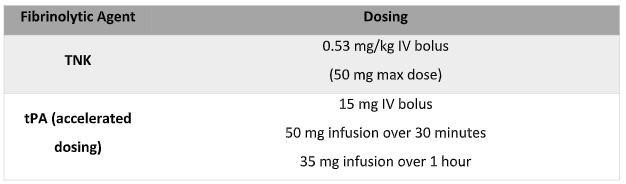
- Recommended dosing schedules for the various fibrinolytic agents:
*If the patient is older than 75 years, consider using half-dose fibrinolytics to mitigate bleeding risk.
- Following fibrinolytic therapy, rapid transfer to a PCI-capable centre is recommended. Patients will receive:
- Immediate PCI for those who failed reperfusion on ECG (failure to achieve > 50% ST-segment resolution in the ECG lead with maximal ST elevation, and/or persistent chest pain/hemodynamic/electrical instability). Ideally 60-90 min post-fibrinolysis.
- Urgent angiography with or without PCI within 24 hours for those with successful fibrinolysis.
- Facilitated PCI (the administration of adjuvant fibrinolytics with or without glycoprotein (GP) IIb/IIIa inhibitors while in transit for PPCI) is not recommended when access to PPCI is available within 120 min of FMC.
Adjunctive Therapy to Fibrinolytics
Aspirin (ASA)
- Loading dose: 162 – 325 mg. If vomiting, administer rectally.
- Duration: 81 mg daily continued indefinitely.
Clopidogrel
- Loading dose: 300 mg PO if patient ≤ 75 years old, 75 mg PO if patient > 75 years old.
- Duration: 75 mg PO daily continued for at least 14 days and up to one year.
Unfractionated heparin (UFH) OR Enoxaparin
UFH
- IV bolus of 60 U/kg (maximum 4000 U) followed by an infusion of 12 U/kg (maximum 1000 U) per hour, adjusted to obtain an aPTT of 1.5 to 2.0 times control.
- Duration: 48 hours or until revascularization.
Enoxaparin
- If age < 75 years: 30 mg INTRAVENOUS bolus, followed in 15 min by 1mg/kg subcutaneously every 12 hours (maximum 100 mg for the first 2 doses).
- If age 75 years: no IV bolus, 0.75 mg/kg subcutaneously every 12 hours (maximum 75 mg for the first 2 doses).
- Regardless of age, if CrCl < 30 mL/min: 1 mg/kg subcutaneously every 24 hours.
- Duration: for index hospitalization, up to 8 days or until revascularization.
Other routine adjunctive therapies may be added after reperfusion, if no contraindications. These include oral beta blockers, statins, and ACE inhibitors.
GP IIb/IIIa inhibitors are discouraged as adjunctive therapies to fibrinolytic therapy because the associated risk of major bleeding outweighs any possible mortality benefit.
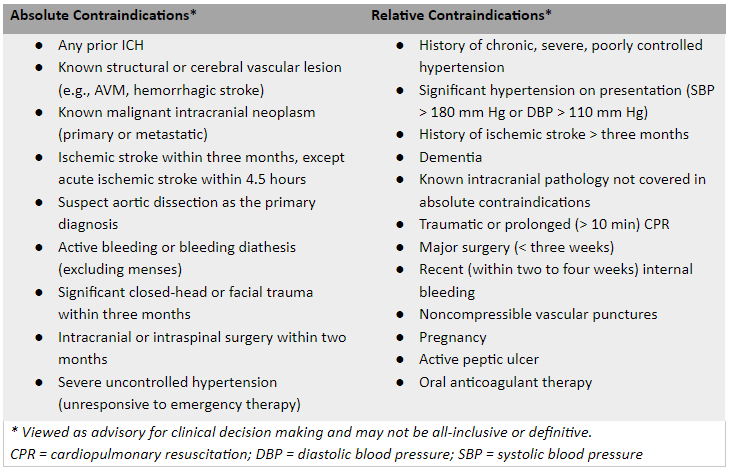
Contraindications to Fibrinolytic Therapy for STEMI
Clinical Decision Making Considerations
- The decision to administer fibrinolytic therapy must weigh the likelihood of potential benefit to that of potential harm and be discussed with the patient prior to use.
- In combination with ASA, fibrin-specific fibrinolytics reduce all-cause mortality by up to 6%.
- Accelerated infusion tPA has an additional reduction in 30-day mortality of 1% when compared to streptokinase. TNK has demonstrated similar mortality benefits as accelerated infusion tPA.
- The baseline risk of intracranial hemorrhage is 0.4% (NNH = 250) and the risk of major non-cerebral bleeds is ~0.7-0.8% (NNH = 137) even without contraindications, and higher if relative contraindications are present.
- Patient factors that may influence the balance of benefit and harm:
- Increased likelihood of benefit: onset of symptoms < 3 hours, significant ischemic territory at risk (anterior or large inferoposterior/right ventricular MI). Overall mortality benefit for large STEMIs is up to 6%.
- Decreased likelihood of benefit: onset of symptoms > 6 hours, smaller ischemic territory at risk (uncomplicated inferior or lateral MI). Small infarcts in younger patients (under 75 years of age) may only gain 1-2% mortality advantage.
- Increased likelihood of major bleeding: age > 75 years, weight < 67 kg, uncontrolled hypertension, renal dysfunction, any other relative contraindication.
Related Information
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Cardiovascular Emergencies
DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 16, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.