Heat-Related Illness
Critical Care / Resuscitation, Environmental Injuries / Exposures
First 5 Minutes
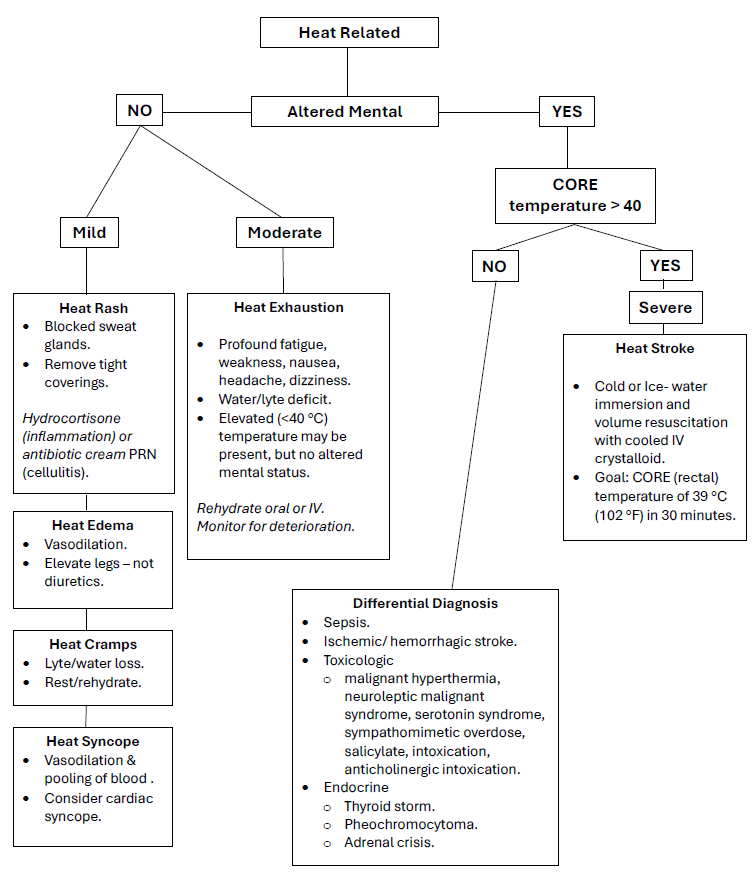
- Heat stroke is life-threatening and is defined as: Core (rectal) temperature > 40°C (104°F) and CNS abnormalities due to exposure to environmental heat (classic heat stroke) or strenuous exercise (exertional heat stroke).
- Rapid cooling in cold-water or ice-bath to obtain Core temp 38-39 ideally within 30 minutes is goal.
- Rehydration is critical.
- Consider other causes of hyperthermia – sepsis, thyroid storm, serotonin syndrome, neuroleptic malignant syndrome, Aspirin overdose, sympathomimetic use, etc.
Context
- Heat-related illness is a spectrum of disease from heat edema, cramps, syncope, exhaustion to heat stroke.
- A multisystem, life-threatening illness characterized by elevation of the core body temperature (to > 40°C) and CNS dysfunction due to thermoregulatory failure and cardiovascular collapse – pathophysiology still unclear.
- Heat stroke can lead to multiorgan failure (renal failure, rhabdomyolysis, electrolyte abnormalities: hyperglycaemia, low phosphate) with mortality rate of 60% in classic heat stroke (30% in exertional.)
- Classic heat stroke occurs in patients with preexisting conditions.
- Exertional heat stroke involves healthy persons with increased metabolic heat generation through physical exertion, often but not necessarily with heat exposure, e.g., athletes, those working in hot environments (outside and inside), concert/festival attendees, etc.
- Risk of heat related illness: heat exposure (environmental or internally-generated), individual susceptibility (age, comorbidities and medication, substance use) and socioeconomic factors (lack of access to health care and community care-cooling centers.)
Diagnostic Process
Recommended Treatment
- Focus usually on cardiovascular resuscitation and correction of body temperature and fluid & electrolytes including glucose.
- Myocardial dysfunction may necessitate inotropes or even ECMO, if available.
- Active cooling to 39°C (cool environment, ice water packs, ice water lavage, cold IV fluids, fans, dialysis.)
- Avoid antipyretics as do not decrease temperature and may add to organ failure.
- No role for pharmacologic therapy in exertional heat stroke.
- May require sedation (benzodiazepines, ketamine) and paralysis (avoid succinylcholine if possible.)
- Treat rhabdomyolysis with crystalloids to achieve urine output > 2-3mL/kg/hr.
Criteria For Hospital Admission
Patients suspected to have a severe heat illness (i.e., heat stroke) and/or signs of hemodynamic instability should be admitted for a period of observation and monitoring for complications.
Criteria For Close Observation And/or Consult
Heat Syncope if cardiac cause suspected.
Heat exhaustion – duration not known but will likely vary from patient to patient (4-6 hours.)
Criteria For Safe Discharge Home
- Depend on clinical presentation and patient’s progress during hospitalization.
- For patients who recover rapidly from exertional heat stroke with cooling and have no residual symptoms, discharge after observation for up to six-hours.
Context
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
- Cold water immersion is the optimal cooling method for heat stroke.
- Target temperature for cooling heat stroke patients should be not be less than 39°C.
- Rectal temperature is the most accurate measurement of core hyperthermia compared to axillary, oral, or aural thermometry.
- Cold intravenous fluids (4°C) should be used adjunctively in cooling heat stroke patients.
- Evaporative or convective cooling can be considered as adjunct cooling methods if cold water immersion is unavailable.
- Dehydration should be minimized in heat illness.
- Ice packs should be applied to cover the entire body.
- Antipyretics should be avoided in heat illness.
- There is currently no role for routine treatment of exertional heat stroke with dantrolene.
Related Information
OTHER RELEVANT INFORMATION
- HealthLinkBC: https://www.healthlinkbc.ca/healthlinkbc-files/heat-related-illness (15 Languages)
- VIDEO (June 2024) “Overview of Heat-Related Illness – NEJM”: https://www.youtube.com/watch?v=PQ9iJKnkO5I
Reference List
Atha, W. F. (2013). Heat-related illness. Emergency medicine clinics of North America, 31(4), 1097-1108.
Rublee C, Dresser C, Giudice C, Lemery J, Sorensen C. Evidence-Based Heatstroke Management in the Emergency Department. West J Emerg Med. 2021 Feb 26;22(2):186-195. doi: 10.5811/westjem.2020.11.49007. PMID: 33856299; PMCID: PMC7972371.Cheshire Jr, W. P. (2016). Thermoregulatory disorders and illness related to heat and cold stress. Autonomic Neuroscience, 196, 91-104.
Grubenhoff, J. A., du Ford, K., & Roosevelt, G. E. (2007). Heat-related illness. Clinical Pediatric Emergency Medicine, 8(1), 59-64.
Lipman, G. S., Gaudio, F. G., Eifling, K. P., Ellis, M. A., Otten, E. M., & Grissom, C. K. (2019). Wilderness Medical Society Practice Guidelines for the Prevention and Treatment of Heat Illness: 2019 Update. Wilderness & Environmental Medicine.
O’Connor, F. G., Casa, D. J. (2019). Exertional heat illness in adolescents and adults: Management and prevention. In J. Grayzel (Ed.), UpToDate. Retrieved November 11, 2019, from https://www.uptodate.com/contents/exertional-heat-illness-in-adolescents-and-adults-management-and-prevention
Pryor, R. R., Casa, D. J., Holschen, J. C., O’Connor, F. G., & Vandermark, L. W. (2013). Exertional heat stroke: strategies for prevention and treatment from the sports field to the emergency department. Clinical Pediatric Emergency Medicine, 14(4), 267-278.
Sorensen C, and Hess J. Treatment and Prevention of Heat-Related Illness. N Engl J Med 2022;387:1404-13. DOI: 10.1056/NEJMcp2210623
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jul 09, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.