Hyperkalemia – Diagnosis and Treatment
Cardinal Presentations / Presenting Problems, Metabolic / Endocrine
First 5 Minutes
In known or suspected hyperkalemia:
- Initiate cardiac monitoring.
- Obtain IV access.
- Order an ECG and a lab re-draw.
- If hyperkalemic emergency (defined below), initiate calcium, insulin and dextrose.
Context
Hyperkalemia is defined as serum K+ >5.2 mmol/L
– Can provoke dangerous arrhythmias and ultimately cardiac arrest in severe cases.
Common causes of significant hyperkalemia include:
- Increased K+ release from cells (intracellular à extracellular shift.)
- Pseudohyperkalemia (hemolyzed sample, extremely common.)
- Metabolic acidosis via H+ exchange.
- Insulin deficiency, hyperglycemia, hyperosmolality.
- Increased tissue catabolism, exercise (e,g., rhabdomyolysis.)
- Decreased excretion.
- AKI/CKD
- Decreased aldosterone secretion or sensitivity (i.e., RAAS blockade via ACEs, ARBs.)
- Reduced renal sodium and water delivery (i.e., effective arterial blood volume depletion.)
Diagnostic Process
Signs and symptoms:
- Usually asymptomatic.
- If moderate to severe hyperkalemia, can variably see:
- CVS: Arrhythmias
- Neuromuscular: muscle cramps, generalized weakness, paresthesias, tetany, focal or global paralysis
- GI: nausea, vomiting, diarrhea
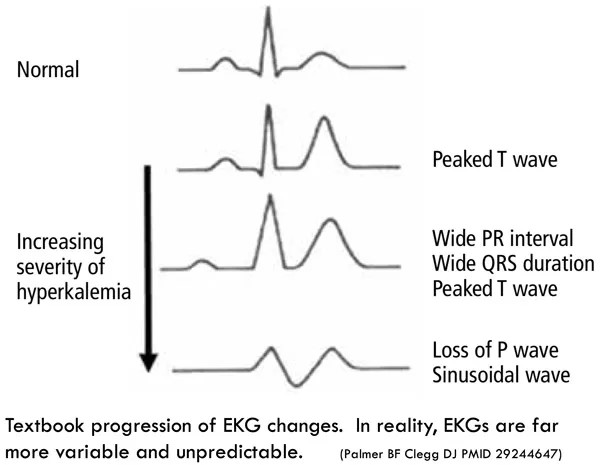
ECG findings:
- Hyperkalemia can lead to nearly any cardiac arrhythmia.
- “Typical” findings are not sensitive or specific – can be absent in very high K+, or can be present in normal K+ for other reasons.
- Typical findings include:
- Tall-peaked T waves
- Wide PR interval
- Shrinking and then loss of P waves
- Widening of the QRS interval à Sinusoidal Wave
Recommended Treatment
Approach to treatment in the ED:
- Determine if hyperkalemic emergency:
– If any of the following, require rapidly acting therapy with calcium and insulin/glucose immediately, followed by K+ removal therapies.
- 1 clinical manifestation of hyperkalemia (muscle weakness or paralysis, cardiac conduction abnormalities or arrhythmias.)
- Serum K+ >6.5 mEq/L
- Serum K+ >5.5 mEq/L with both:
- Significant kidney function impairment
- Ongoing tissue breakdown (e.g., rhabdomyolysis, crush injury, tumour lysis syndrome) or ongoing K+ absorption (e.g., significant GI bleeding.)
- If not hyperkalemic emergency but K+ >5.5 mEq/L and severe kidney function impairment, lower over 6 to 12 hours – rapid acting therapies not required.
- Patients with ESKD or oliguria: Dialysis if available or GI cation exchanger if not.
- Reversal of cause if known (e.g., d/c RAAS blockade.)
- If metabolic acidosis present, treat with bicarbonate.
- If hypervolemic, diurese.
- If none of the above (K <5.5 mEq/L, or >5.5 mEq/L but preserved renal function) K+ can be lowered slowly (ex. dietary modification, diuretics, bicarbonate, reversal of causes (e.g, NSAIDS, hypovolemia) etc.)
Treatment modalities:
- Myocardial stabilization
- Calcium gluconate 10 mL of 10% solution (1g of calcium) infused over 2-3 minutes. Repeat after 5 minutes if ECG changes persist on cardiac monitoring.
-
- Duration of action is 30-60 minutes, can be repeated q30-60mins if non-resolving and not hypercalcemic.
- Shift K+ to intracellular compartment
- Insulin/Dextrose: 10 units of rapid insulin bolused with 50mL of D50W over 5 minutes, then D10W at 50 – 75 mL/hr
- Can hold dextrose if glucose >13.9 mmol/L.
- Monitor glucose q1h x 6 hours to ensure no hypoglycemia
- Bicarbonate: 100mL of 8.4% HCO3-
- Adjuvant therapy if concurrent metabolic acidosis
- Salbutamol: 0.5mg IV or 20mg albuterol nebulized
- Adjuvant therapy only
3. Eliminate K+ from body
Diuretics (if reasonable kidney function)
- Hypervolemia: furosemide 40mg IV q12h
- Euvolemic or hypovolemia: Achieve euvolemia with Lactated Ringers (see reference 5) first, then furosemide 40mg IV q12h + continuous LR to maintain volume status.
K+ binders (gastrointestinal cation exchanger)
-
- Sodium zirconium cyclosilicate 10 g po or patiromer 8.4 g po can be given, especially in patients with severe kidney function impairment in whom hemodialysis cannot be quickly performed.
- Do not use sodium polystyrene sulphonate (kayexalate) unless there are no other options due to risk of adverse events and lack of evidence for efficacy.
Dialysis
- Essential therapy in patients with ESKD or severe kidney function impairment.
Criteria For Hospital Admission
- Patients with hyperkalemic emergency should be admitted to hospital.
- Any clinically unstable patient with hyperkalemia requires admission to ICU setting
- All moderate or severe hyperkalemia cases should be admitted as a monitored inpatient during and after treatment.
Criteria For Transfer To Another Facility
- In patients requiring dialysis, transfer may be necessary depending on availability of dialysis.
Criteria For Close Observation And/or Consult
- Patients who receive insulin should undergo hourly glucose measurements for 6 hours to monitor for hypoglycemia.
- Patients with hyperkalemic emergency in the setting of ESKD should have urgent nephrology consult.
Criteria For Safe Discharge Home
- Hyperkalemia resolved, etiology discovered and addressed, with follow up plans arranged as necessary.
- If on RAAS blockade, follow up with prescribing provider to adjust as necessary.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Kayexalate has significant potential for harm without significant benefit in management of hyperkalemia and should not be used unless no other options: High quality evidence based on decades of studies, and FDA recommendations.
- Lactated ringer’s is preferred to normal saline for volume resuscitation in hyperkalemia: Moderate quality evidence based on multiple double-blinded, replicated trials, though with somewhat small sample sizes.
Related Information
OTHER RELEVANT INFORMATION
Hyperkalemia ECGs: https://litfl.com/hyperkalaemia-ecg-library/
Lactated ringers in hyperkalemia: https://emcrit.org/pulmcrit/myth-busting-lactated-ringers-is-safe-in-hyperkalemia-and-is-superior-to-ns/
Use of kayexalate: https://rebelem.com/kayexalate-useful-treatment-hyperkalemia-emergency-department
Related Information
Reference List
David M. Treatment and prevention of hyperkalemia in adult. In: UpToDate [Internet]. 2022. Available from: https://www.uptodate.com/contents/treatment-and-prevention-of-hyperkalemia-in-adults
Littmann L, Gibbs MA. Electrocardiographic manifestations of severe hyperkalemia. J Electrocardiol. 2018;51(5):814–7.
Long B, Warix JR, Koyfman A. Controversies in Management of Hyperkalemia. J Emerg Med. 2018 Aug;55(2):192–205.
Pfennig CL, Slovis CM. Chapter 125. Electrolyte Disorders. In: Marx JA et al. eds. Rosen’s Emergency Medicine, 8e. Philadelphia: Elsevier Saunders; 2014.
Farkas J. Myth-busting: Lactated Ringers is safe in hyperkalemia, and is superior to NS. [Internet]. EMCrit Project. 2014 [cited 2022 Dec 1]. Available from: https://emcrit.org/pulmcrit/myth-busting-lactated-ringers-is-safe-in-hyperkalemia-and-is-superior-to-ns/
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 16, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.