Intercostal Nerve Block
Respiratory, Trauma
Context
- Indications for intercostal nerve blocks include rib fractures, herpes zoster, intercostal neuralgia, malignant processes involving the thorax, post-traumatic and post operative pain, and breast surgery and upper abdominal surgery anesthesia.
- The only absolute contraindication is infection over the site where LA would be injected. Relative contraindications include anticoagulation, coagulopathy diagnosis or previous nerve damage at the site where the block would occur.
- Complications include pleural effusion, local anesthetic toxicity and hemothorax, all of which are rare.
- Incidence of pneumothorax has been found to be between 0.073% and 19%, although a retrospective chart review found that the incidence was 1.4% for each individual nerve blocked.
- Intercostal nerve blocks reduce the need for narcotics and improve lung rehabilitation, thereby reducing pulmonary complications.
- Intercostal nerve blocks improve pain for 6 – 10 hours when done correctly and provide a one-sided analgesia along the dermatomal distribution for the vertebral level where they are done.
- Intercostal nerve blocks can be conducted more easily than paravertebral nerve blocks or epidurals but there is increased risk of vascular uptake relative to the other procedures.
Anatomy
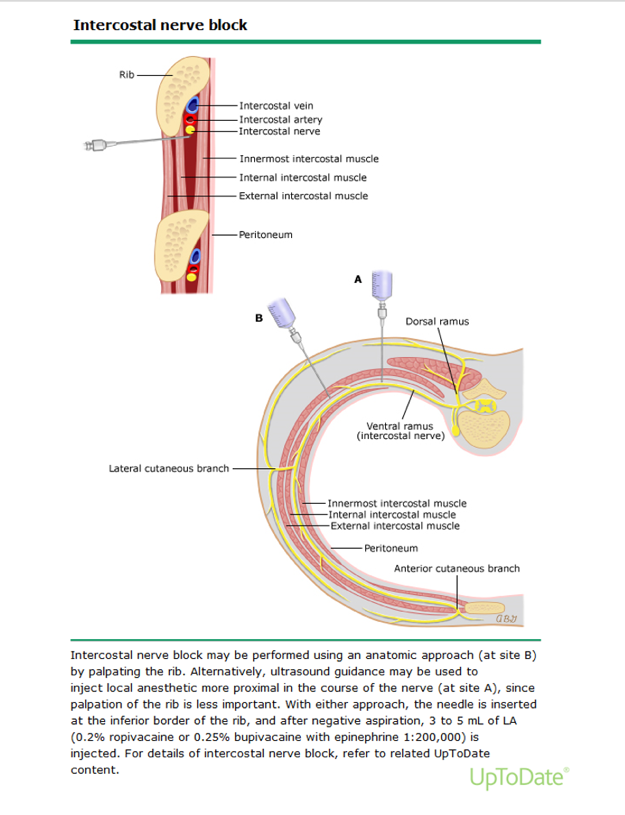
- Spinal nerves T1 to T11 divide into ventral and dorsal rami.
- The ventral rami become the intercostal nerves when they enter the groove on the underside of each rib.
- The intercostal nerves travel along the underside of each rib, and make up the most inferior portion of the neurovascular bundle.
- T1 to T7 are the thoracic intercostal nerves and T8 to T11 are the thoracoabdominal intercostal nerves.
- The thoracic intercostal nerves innervate the parietal pleura with its lateral and anterior branches innervating the skin of the thorax.
Equipment
Skin antiseptic, sterile gauze, local anesthetic, sterile gloves, 22 – 25 gauge needle (50 mm long), marking pen, ECG monitor, BP monitor, pulse oximetry.
Anatomical Landmark-guided Technique
- The block can be done anywhere along the course of the intercostal nerve that is proximal to the midaxillary line.
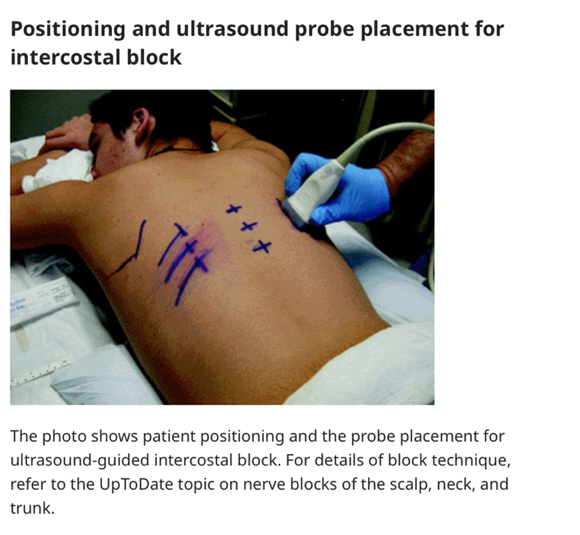
- Patients are placed in prone position, lateral decubitus position or sitting position (where they lean forward to pull the scapula laterally).
- Ribs are blocked at around 6-8 cm from the midline in most adults.
- A 22 – 25-gauge needle (50 mm long) is pointed cephalad at an angle of around 20 degrees in the sagittal plain. After approximately 1 cm, the inferior rib is reached at which point the needle should be moved off the rib surface, pushed 1 – 3 mm anterior before aspirating to ensure needle is not in vascular space.
- Inject 3 – 5 mL of anesthetic (0.2% ropivacaine or 0.25% bupivacaine with epinephrine 1: 200,000) in the intercostal groove inferior to the rib.

Ultrasound-guided Intercostal Nerve Block
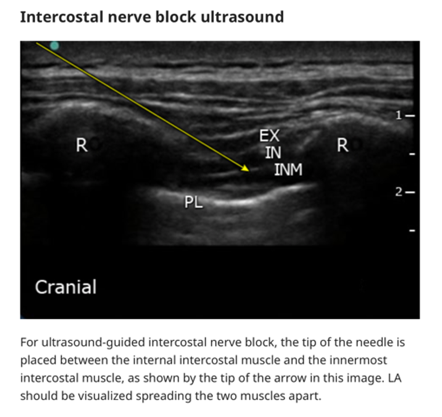
- Decreased risk of intravascular injection or pneumothorax relative to approach using only anatomical landmarks.
- Because injection can be done closer to the vertebrae when using ultrasound, it allows for more reliable injection prior to the intercostal nerve’s division into lateral and anterior branches, thereby increasing the surface area of anesthetic coverage.
- The ultrasound transducer is placed 4 cm lateral to the spinous process and the needle should be visualized between the internal intercostal muscle and the innermost intercostal muscle on ultrasound.
- Inject 3 – 5 mL of anesthetic (0.2% ropivacaine or 0.25% bupivacaine with epinephrine 1:200,000).
 For both landmark and ultrasound guided techniques patients should be monitored for 30 minutes afterwards to make sure there’s no delayed absorption of local anesthetic.
For both landmark and ultrasound guided techniques patients should be monitored for 30 minutes afterwards to make sure there’s no delayed absorption of local anesthetic.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
This appears to be a relatively new technique, so there are discrepancies on the approaches used, and limited data on which approaches work best.
Related Information
OTHER RELEVANT INFORMATION
Reference List
Baxter, C., Singh, A., Ajib, F., & Fitzgerald, B. (2021). Intercostal Nerve Block. Statpearls.
Elkhashab, Y., & Wang, D. (2021). A Review of Techniques of Intercostal Nerve Blocks. Current Pain And Headache Reports, 25(10). doi: 10.1007/s11916-021-00975-y
Ho, A., Buck, R., Latmore, M., Levine, M., & Karmakar, M. Intercostal Nerve Block – Landmarks and Nerve Stimulator Technique – NYSORA. Retrieved 3 February 2022, from https://www.nysora.com/regional-anesthesia-for-specific-surgical-procedures/thorax/intercostal-nerve-block/
Shanti, C., Carlin, A., & Tyburski, J. (2001). Incidence of Pneumothorax from Intercostal Nerve Block for Analgesia in Rib Fractures. Journal Of Trauma And Acute Care Surgery, 51(3), 536-539. doi: 10.1097/00005373-200109000-00019
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 02, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.