Major Burns Trauma
Critical Care / Resuscitation, Trauma
Context
- Major burn trauma (MBT) presents many challenges to practitioners because of the complex pathophysiology and the need for multidisciplinary medical and surgical management.
- Prehospital personnel and rural emergency physicians spend an important portion of time with major burn trauma patients, and the care these practitioners provide early in the resuscitation process has a major impact on patient morbidity and mortality later on.
- In light of changing perspectives on burn pathophysiology, the BC Provincial Major Burns Working Group recommends a resuscitation formula of 3 mL/kg/%Total Body Surface Area (TBSA).
- In addition to new concepts in fluid resuscitation for burns, novel therapies such as high dose vitamin C, early colloid administration, and selective use of vasoactive agents to improve perfusion pressures are also gaining traction in complex burn care.
Management
Highlights from the Major Burns Trauma Clinical Practice Guidelines:
- Front-end resuscitation, especially in the first 24 hours, has a significant impact on morbidity and mortality later in a patient’s care. Specifically, front-end over-resuscitation can be as harmful as under-resuscitation. Inadvertent over-resuscitation with crystalloid (beyond 4 mL/kg/%TBSA in the first 24 hours) should be avoided.
- Recommendation: fluid resuscitation for major burns should start at 3cc/kg/%TBSA.
- Recommendation: Perform hourly calculation of “ins” and “outs”. Titrate fluid resuscitation hour-by-hour, especially in the early phase of major burns trauma. Clinical endpoints include responses in blood pressure, heart rate, and lactate clearance. Titrate urine output to 30-50cc/hr for major burns (and 50-100cc/hr in electrical burns).
- Large volume crystalloid resuscitation can propagate and exacerbate acid-base status, coagulopathy, and hypothermia.
- Recommendation: Use warmed, balanced crystalloids (Ringer’s Lactate or Plasmalyte-A) in major burns. Cool the burns, but warm the patient. Consider the selective use of colloids and vasopressors (see note below). Large volume resuscitation with Normal Saline is not recommended.
- Hemodynamically unstable patients are commonly treated with successive fluid boluses, while the use of vasoactive agents was avoided. Inadvertent over-resuscitation with crystalloid (beyond 4 mL/kg/%TBSA in the first 24 hours) can be responsible for significant, preventable contributions to subsequent morbidity and mortality and should be avoided.
- Recommendation: Hemodynamic instability can be mitigated with the selective use of colloids (i.e. 5% or 25% albumin – see Steps 4-5 of CPG) and vasoactive agents (e.g. levophed or norepinephrine).
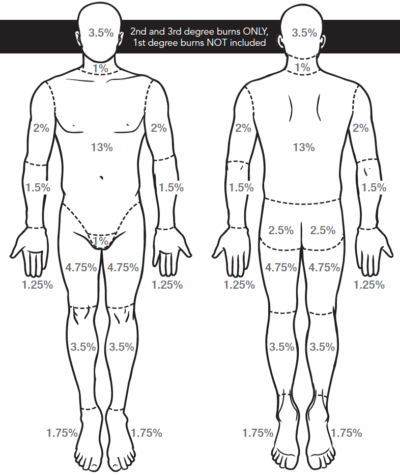
- Fluid resuscitation based on inaccurate %TBSA estimates can lead to complications. Higher rates of abdominal compartment syndrome are noted in patients when %TBSA calculations were overestimated. Furthermore, health care providers estimates of the %TBSA tend to vary widely.
- Recommendation: The Lund-Browder chart yields the greatest accuracy and reproducibility between clinicians. As such, we recommend the use of the Lund-Browder chart for the estimation of %TBSA.
- Cyanide toxicity remains a common confounder in inhalation injury, especially in enclosed-space fires. There are no readily-available bed-side tests to confirm cyanide toxicity.
- Recommendation: Cyanide toxicity should be strongly considered in the proper context: enclosed-space fire and presence of inhalation injury with altered level of consciousness (GCS < 13), profound shock (SBP < 90mmHg), high serum lactic acid (lactate > 10mmol/L), and/or a narrow arterio-venous gradient (PaO2 on an arterial blood gas is similar to the PaO2 on a venous blood gas).
- Recommendation: In confirmed or suspected cyanide toxicity, the hydroxocobalamin (Cyanokit) should be given as soon as possible, at a starting dose of 5 grams (70mg/kg in pediatrics, Pregnancy Category C).
- Airway management with tracheal intubation and positive pressure ventilation is sometimes required when major burn trauma affects the head and neck, and/or in anticipation of respiratory compromise in the context of major resuscitation, critical illness, or anticipated critical care transport.
- Recommendation: Anticipate that all patients who have inhalation injuries or burns to the head and neck will be difficult airways. Back up personnel, alternative intubating devices, and a clear airway management plan are strongly recommended.
- Escharotomy should be considered anytime full thickness circumferential burns are identified; however, the location and extent of burns will guide the immediate versus deferred management. If identified, contact Burn Physician via PTN to discuss the need, timing and preferred technique for escharotomy.
- Dressings:
- Saline soaked gauze is okay.
- Cool the burn but warm the patient. Saline soaked gauze is helpful in stopping the burning process, but when doing so the clinician should also monitor the patient’s core temperature and avoid over-cooling and inducing hypothermia.
- Contact the Burn Physician for guidance on burn wound management during the transport phase.
- Early consultation with a Burn Physician is encouraged.
Criteria for Referral to Burns Centre
Consultation and/or transfer to a burn center should be considered for all acutely burned patients who meet any of the following criteria:
- Partial thickness burns > 20% TBSA in patients aged 10 – 50 years old.
- Partial thickness burns >10% TBSA in children aged 10 or adults aged 50 years old.
- Full-thickness burns > 5% TBSA in patients of any age.
- Patients with partial or full-thickness burns of the hands, feet, face, eyes, ears, perineum, and/or major joints.
- Patients with high-voltage electrical injuries, including lightning injuries.
- Patients with significant burns from caustic chemicals.
- Patients with burns complicated by multiple trauma in which the burn injury poses the greatest risk of morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, the patient may be treated initially in a trauma center until stable before being transferred to a burn center. Physician judgment will be necessary in such situations and should be in concert with the regional medical control plan and triage protocols.
- Patients with burns who suffer inhalation injury.
- Patients with significant ongoing medical disorders that could complicate management, prolong recovery, or affect mortality.
- Hospitals without qualified personnel or equipment for the care of children should transfer children with burns to a burn center with these capabilities.
- Burn Injury in patients who will require special social/emotional and /or long-term rehabilitative support, including cases involving suspected child abuse, substance abuse, etc.
Resource: Major Burns Pre-Transfer Checklist
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Key Contact Information
Major Burns Trauma Clinical Practice Guidelines (see ‘Resources’ section):
BC Emergency Health Services:
- Patient Transfer Network: 604-215-5911 or Toll Free: 1-866-233-2337
- EMS Physician Online Support: 604-215-5911 or Toll Free: 1-866-233-2337
BC Burns Centres:
- Vancouver General Hospital
- Royal Jubilee Hospital
- BC Children’s Hospital (Age < 16 years)
Related Information
OTHER RELEVANT INFORMATION
-
Burns Update: ‘Fireworks with short fuses’. Presented by Dr. Anthony Papp presents at St. Paul’s Emergency Medicine Update, Whistler 2017.
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Nov 26, 2019
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.