Management of agitated patient in the Emergency Department – Adult
Other, Psychiatric and Behaviour, Special Populations
Context
Violence towards health care workers is unfortunately common.
40% of all violence-related claims in BC are submitted by health care workers despite only making up 5% of the workforce.
- Up to 50% of health care workers will experience violence during their careers.
- Violence and agitation = behaviours &/or actions that can cause harm or injury to another person.
- The manifestations of violence and agitation are diverse and depend on a combination of extrinsic (environment, provider attitudes, and behaviour) and intrinsic (medical conditions, personality characteristics, mental distress) factors.
High-risk factors
—associated with agitation and violence include:
-
- Alcohol or drug use disorders.
- Young age.
- Male.
- Personal history of violence.
- Chronic pain.
- Poor communication among staff.
- Lack of privacy.
Signs of impending violence
-
- Angry demeanor.
- Loud/aggressive speech.
- Provocative behaviour.
- Tense posturing.
- Pacing or frequently changing body position.
☎ Call the police
—immediately if:
-
- Acts destructively (ie. hitting things or destroying equipment).
- Is armed,
- Makes verbal or physical threats that you do not have the resources (security) to contain,
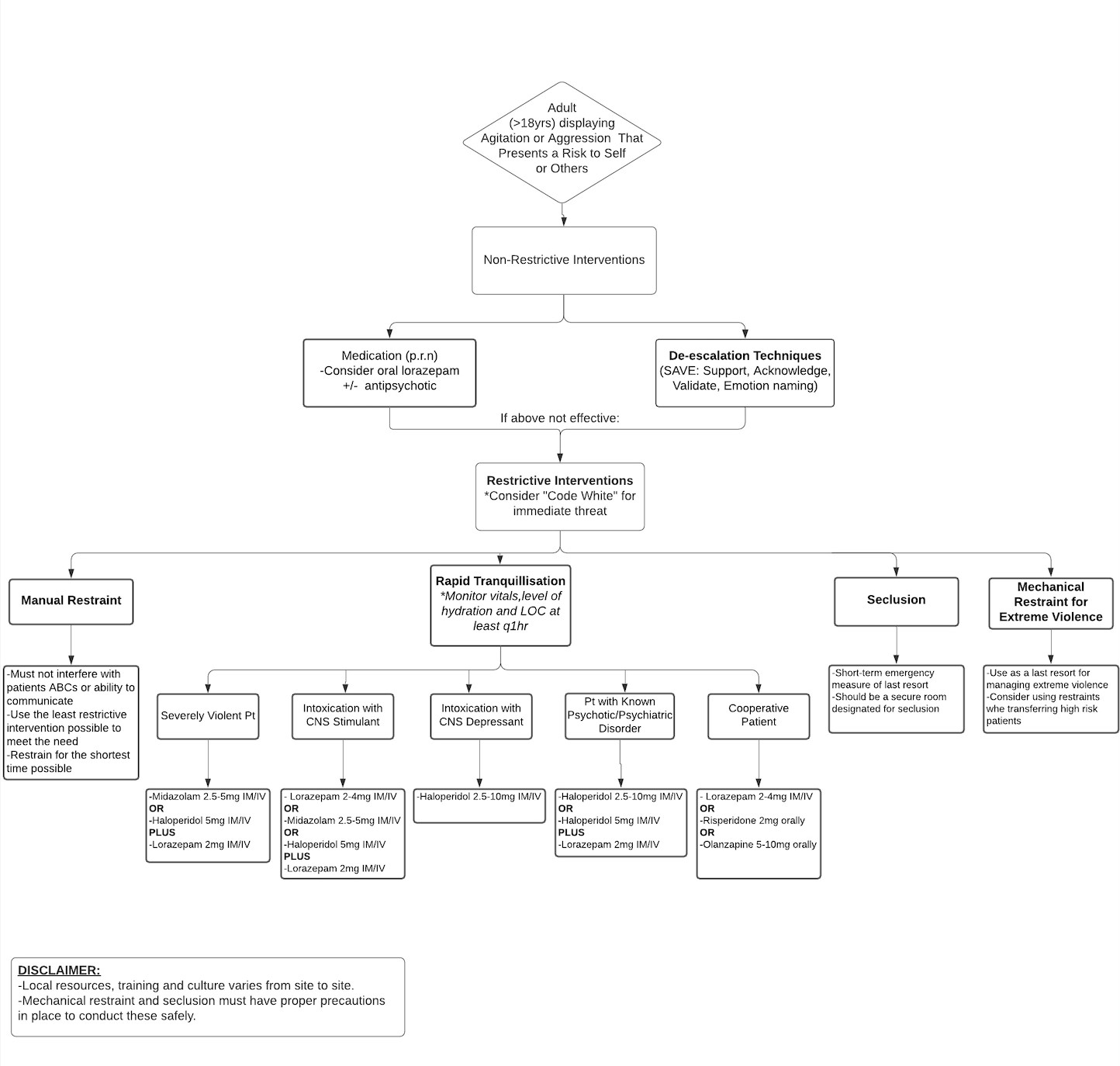
Recommended Treatment
Criteria For Hospital Admission
- If an underlying psychiatric or medical condition has been identified and requires inpatient management.
- Patients should be observed post-sedation for further assessment and monitoring.
- Degree of sedation (Glasgow coma scale).
- Vitals.
- Pupils.
- Blood glucose.
- ECG rhythm.
- Adverse effects of antipsychotic meds: Neuroleptic Malignant Syndrome (NMS), extrapyramidal symptoms, hyperprolactinemia, postural hypotension, serotonin syndrome (link between SGAs and serotonin syndrome).
Observe patients in alcohol withdrawal
1/20 people with withdrawal symptoms may experience delirium tremens (DT)—increased risk of heart attack, stroke, or death.
Criteria For Close Observation And/or Consult
Level of Observation
—consider patient’s:
- Current mental state.
- Risk assessment.
- Medications and side effects.
Views of the patient:
-
- Low-level intermittent observation = every 30-60 mins.
- High-level intermittent observation = every 15-30 mins.
- Use in patients where there is no immediate risk, but you suspect they could become violent or aggressive.
- Continuous observation: if patient presents immediate threat.
- Multiprofessional continuous observation: highest risk patients. Need to be within eyesight of 2 or 3 staff.
Criteria For Safe Discharge Home
- Consider discharge in patients where the underlying concern has resolved.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Moderate: Recommendations come from clinical guidelines and articles, which are in relative agreement on the management of agitation in the Emergency Department.
Related Information
OTHER RELEVANT INFORMATION
-
-
-
GUIDELINES: CODE WHITE RESPONSE. A Component of Prevention and Management of Aggressive Behaviour in Healthcare.
Albach D. , Armstrong J. , Bullock L., et all.
Health Association of BC. | Work Safe BC | Occupational Health and Safety Agency for Healthcare in BC.
www.saswh.caPreventing Violence in Health Care: Five Steps to an Effective Program.
Work Safe BC (Dec 2005).
worksafebc.com/
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Patient Safety and System Resilience in Emergency CareRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Apr 27, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.