Neuroleptic Malignant Syndrome (Diagnosis & Treatment)
Cardinal Presentations / Presenting Problems, Critical Care / Resuscitation, Neurological, Psychiatric and Behaviour, Toxicology
Context
- Neuroleptic malignant syndrome (NMS) is rare, but life threatening and often overlooked.
- Associated with new onset, increased dose, or combination of antidopaminergic drugs such as antipsychotics or metoclopramide, or the withdrawal of Parkinson disease medications.
- Four cardinal features: altered mental status, severe “lead pipe” rigidity, fever (often above 40deg), and autonomic instability (hypertension, tachycardia).
- Associated mortality of 5.6%.
Diagnostic Process
Clinical manifestations
- Classically four defining features of NMS, developing over days, often in the following order:
- Altered mental status: Often the initial symptom, frequently underappreciated. May present as simple agitation, delirium, or may be profoundly obtunded.
- Muscle rigidity: Severe, bilateral muscle rigidity. Rigidity is described as “lead-pipe” and is smooth throughout range of motion (versus cogwheeling). There may be other extrapyramidal symptoms including tremor, dyskinesia, dystonia.
- Fever: Common to have a temperature above 40 degrees.
- Autonomic instability: Primarily sympathetic symptoms including hypertension, tachycardia, tachypnea, diaphoresis (often severe).
Investigations
- Lab work should include basic CBC and chemistry, creatinine, LFTs, CK, tox screen, blood gas, and cultures ± CSF analysis, to rule out competing diagnoses.
- CK often elevated (above 1000) in the context of muscle rigidity leading to rhabdomyolysis.
- Creatinine may be elevated as a consequence of rhabdomyolysis.
- Other non-specific findings: Leukocytosis, hypo/hypernatremia, hyperkalemia, hypocalcemia, hypomagnesemia.
Diagnosis
- Diagnosis is largely based on clinical suspicion based on history of antipsychotic dose changes, clinical presentation, and examination, supported by laboratory markers (elevated CK).
- No diagnostic gold standard exists.
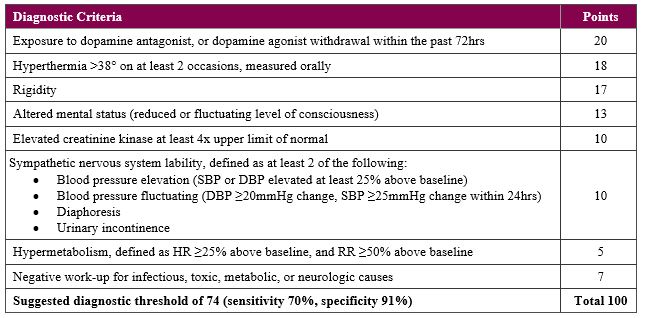
- One diagnostic tool has been proposed (below), though notably, the absence of meeting the diagnostic threshold does not rule out NMS as its presentation may be atypical or its features may continue to develop over time.
- Importantly, the diagnosis should be considered early to initiate treatment before all the diagnostic criteria are met.
Differential diagnosis
Recommended Treatment
Stop the offending agent
- Discontinue any antipsychotics or dopamine acting anti-emetics (metoclopramide).
- If recent withdrawal of Parkinson’s disease medications, restart these medications.
Protect the airway
- May require intubation and higher level of care if significantly obtunded.
Provide supportive care
- Treat hyperthermia with antipyretics and external cooling (cooling blankets, evaporative cooling, ice packs).
- Provide fluids to treat rhabdomyolysis and prevent renal injury. Correct insensible losses of volume.
- Lower blood pressure if markedly elevated.
- Correct electrolyte abnormalities.
- Provide DVT prophylaxis given significant immobility and rigidity.
Benzodiazepines
- Benzodiazepines can control agitation and allow for muscle relaxation.
- Usual dose: lorazepam 1-2mg IV q8hrs as needed.
Specific treatments
- Controversy exists whether dantrolene and bromocriptine are effective, and randomized controlled trials are lacking.
- Their use is primarily supported by their pharmacological effect and various case reports/anecdotes suggesting that these agents cause more rapid clinical improvement and faster overall resolution. However, this is debated in the literature.
- Dantrolene 1-2.5mg/kg IV, may repeat 1mg/kg q6h x 48h (max 10mg/kg/day)
- Works as a skeletal muscle relaxant by inhibiting calcium release in myocytes.
- May cause hepatotoxicity and LFTs should be monitored.
- Bromocriptine 2.5mg PO/NG q8-12h, titrated to a max of 45mg/day
- Works as a dopamine agonist, restoring lost dopaminergic tone.
- Continue therapy for 10 days after NMS is controlled, then taper slowly.
- Monitor for hypotension and CNS depression. May exacerbate psychosis by worsening hallucinations.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The NMS diagnostic tool has moderate sensitivity and high specificity for NMS when a threshold of 74/100 is used.
Dantrolene and/or bromocriptine may improve time to clinical response and time to resolution of NMS.
Related Information
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Sep 06, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…



POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.