Opioid Poisoning – In-Hospital Management
Analgesia / Sedation, Cardinal Presentations / Presenting Problems, Critical Care / Resuscitation, Special Populations, Substance Use, Toxicology
First 5 Minutes
- In addition to presentations with clear substance use history, suspect in any person “found down” or with “decreased level of consciousness”.
- If the patient apneic or lacking adequate ventilatory effort
- Provide assisted ventilation (BVM usually sufficient).
- Administer naloxone.
- If naloxone ineffective, repeat dose every 2-3 minutes until effect.
- Check glucose and address as needed.
- BC Drug and Poison Information Centre if needed: 1-800-567-8911 or
604-682-5050.
Context
- Ultrapotent opioids such as fentanyl are now ubiquitous and may also be found in non-opioid illicit substances such as amphetamines and cocaine. Many illicit opioids also contain additional adulterating substances, which can cause complex drug poisoning presentations.
Diagnostic Process
- Opioid toxidrome, history of substance use, paraphernalia found with the patient, and response to naloxone.
Signs & Symptoms
- Usually presents as sedation, miosis with progression to respiratory depression, coma, and death.
- Possible features of complex opioid poisoning:
- Fentanyl-induced muscle rigidity: clenched jaw, rigid chest / torso, decorticate posturing, standing / unable to sit down, fixed / staring gaze.
- Seizures.
- Dyskinesia.
- Acute lung injury.
- Bradycardia, QT prolongation, Torsades de Pointes.
- Rapid onset following injection or insufflation.
- Peak effect within 1 hour of ingesting regular-release products or crushed/adulterated sustained-release tablets.
- Effects delayed (12-24 hours) with massive ingestion and sustained-release products.
- Effects may be delayed up to 24 hours with ingested fentanyl patches.
Duration of Opioid Effect
- The duration of action depends on dose, ongoing absorption, and the half-life.
- Duration of action in overdose can be significantly longer than therapeutic dosing.
- Short/moderate half-life (2-4 hours):
- Heroin,
- Morphine,
- Hydrocodone
- Hydromorphone,
- Oxycodone,
- Meperidine, and
- Fentanyl* (duration of action of fentanyl may exceed 24 hours in overdose).
- Long half-life (>12 hours):
- Buprenorphine,
- Methadone,
- Loperamide (only absorbed to significant degree in very large OD or with concomitant use of p-glycoprotein inhibitors),
- Oral extended-release preparations.
Recommended Treatment
Supportive Care
- Supplemental oxygen with assisted ventilations as required.
- Protect airway as needed.
- Do not induce vomiting.
- Consider activated charcoal if oral ingestion within 1-2 hrs & no concern for aspiration.
- Hypotension typically responds to IV fluids.
Diagnostics
- Chest x-ray if persistent low O2 sats, abnormal chest sounds or fever.
- Obtain an EKG to rule out significant QT prolongation or other dysrhythmias if methadone or loperamide (an antidiarrheal medication, sometimes used in large doses for opioid effects) is suspected.
Naloxone
Indications
- Respiratory rate persistently < 10 /min.
- Saturation persistently < 92% on room air O2.
- Inability of patient to protect their airway.
- Fentanyl induced chest wall rigidity.
[Note on GCS: GCS may enter into clinical decision making but should not be used on its own as an indication to give additional naloxone. Many patients with co-intoxications have GCS <8 but still maintain an adequate respiratory effort and may not require additional naloxone.]
Goals of Naloxone
- Patient adequately ventilating & oxygenating but not necessarily awake.
- No acute withdrawal symptoms precipitated.
Routes: IV/IO preferred. IM/SC otherwise.
- Note: Naloxone administration alone not an indication to place IO. Only use IO if IO present for other indications. Use IM if no IV/IO present.
Dosing (use lowest effective dose):
- Adults: 0.1 mg IV/IO or 0.4 mg IM if no IV/IO.
- Pediatrics: 0.1 mg/kg IV/IO/IM of body weight.
- If insufficient response, subsequent IV doses should be administered every 2 minutes IV or every 3 minutes IM in escalating doses: 0.4 mg, 0.8 mg, 2.0 mg, 4.0 mg, and then 10 mg as a final dose if there is a high clinical suspicion of opioid intoxication.
- If no response after repeated dosing, look for alternate causes for symptoms (may require airway management).
Naloxone Infusion:
- Consider infusion if multiple naloxone doses required after initial reversal.
- Bolus, then 0.4-0.8 mg/hr titrated to clinical effect.
- Infants = 0.04-0.16 mg/kg/hr.
- Alternatively, administer two-thirds of the initial effective bolus dose per hour to keep the patient maintaining an adequate respiratory effort.
Observation:
- Some patients may be unwilling to stay for prolonged observation periods in the ED. All patients should be informed of the importance of monitoring due to possibility of opioid toxicity recurrence after initial naloxone reversal.
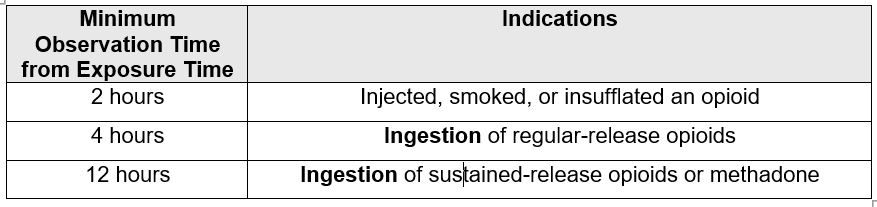
- Patients who have NOT required any naloxone:
- Patients who have required any naloxone:
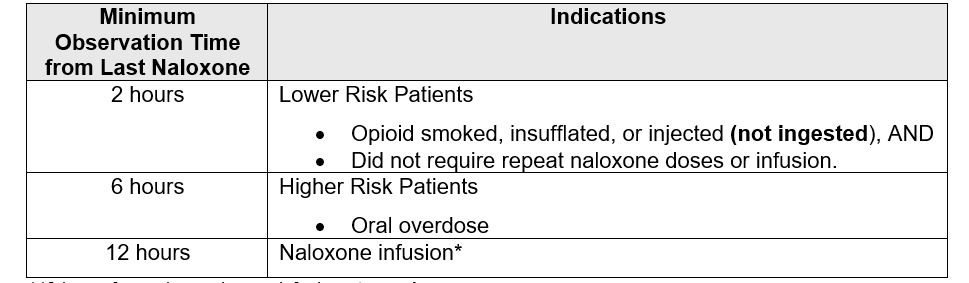
*12 hours from when naloxone infusion stopped References: BCCDC Naloxone Decision Support Tool and BC Drug and Poison Information Centre 2017 Opioid Overdose Best Practices Guideline
Criteria For Hospital Admission
- Acute lung injury.
- Inadequate response to antidote therapy.
- Ongoing naloxone infusion needed.
Criteria For Transfer To Another Facility
- If patient requires ICU care not available locally.
Criteria For Close Observation And/or Consult
- Toxicology consult should be obtained for all pediatric or body packing/stuffing exposures as well as any supratherapeutic exposure to methadone, buprenorphine or fentanyl patches.
- Consider Toxicology consult if non-response to usual care and/or complicated co-intoxication.
- BC Drug and Poison Information Centre 604-682-5050, or 1-800-567-8911.
Criteria For Safe Discharge Home
- Awake, alert with normal vital signs and oxygen saturation on room air and can mobilize as usual without verbal or physical stimulation.
- Offer patients take-home naloxone, safer consumption supplies & access to addictions services at discharge. Harm Reduction | Transition to Care
Related Information
OTHER RELEVANT INFORMATION
BC Drug and Poison Information Centre Opioid Overdose Best Practices Guideline
BCCDC Naloxone Decision Support Tool
For more in-depth review:
- VCH SURKit: Substance Use Response Kit
- Take Home Naloxone – naloxonetraining.com Tool for patients to learn how to use a Take Home Naloxone Kit. It can also be used in centres where staff members are not very familiar with dispensing THN.
- ECBC Harm Reduction in the ED
- ECBC Language Matters
Reference List
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jul 16, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.