Pericarditis – Diagnosis
Cardiovascular, Inflammatory
Context
- True incidence of pericarditis unknown: 5% of non-ACS “chest pain” ED visits.
- Cardiac tamponade can occur in up to 15% of cases.
- Important to distinguish from ACS.
- Inflammatory condition of the pericardium:
- Infectious etiologies
- Most common cause is viral or idiopathic as etiologic agent is rarely identified.
- Consider tuberculosis if recent travel to an endemic region.
- Non-infectious etiologies
- Autoimmune conditions – SLE, RA, scleroderma, sarcoid, vasculitis.
- Autoinflammatory pericardial syndromes (Dressler syndrome): post myocardial infarction, cardiac surgery or cardiac trauma.
- Neoplastic: (metastatic: lung>breast>leukaemia and lymphoma>melanoma).
- Radiation.
- Metabolic (uremia).
- Drug-related.
- Symptoms usually last 4-6 weeks but other forms exist
- Incessant pericarditis: up to 3 months.
- Recurrent/relapsing pericarditis: symptoms recur after a symptom-free period.
- Chronic pericarditis: symptoms > 3 months.
- Infectious etiologies
Clinical Presentation
History
- Quick onset, sharp chest pain:
- Pleuritic – worse on inspiration
- Improves with sitting and leaning forward
- May radiate to neck, back, shoulder and/or jaw
- May be preceded by a gastrointestinal or “flu-like” syndrome.
Physical Examination
- Tachycardic, tachypneic, fever
- Friction rub highly specific but only present in 30% of cases
- Can fluctuate hourly.
- Heard best at end expiration, with the patient leaning forward.
ECG
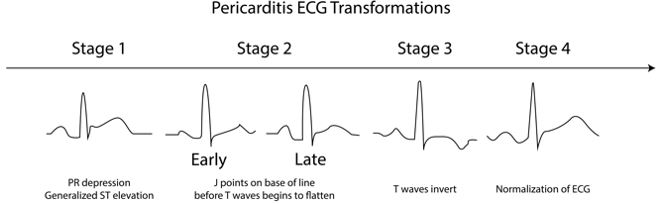
- There are four stages of ECG evolution in pericarditis, all of which are found in 60% of cases (figure 1).
- Stage 1 (hours to days): Diffuse ST elevation and PR depression, ST depression in aVR only
- Stage 2 (within first week): ST and PR segments normalize
- Stage 3: Diffuse T wave inversion and ECG otherwise normal
- Stage 4: T waves return to normal (May have indefinite persistence of T wave inversion)
Created By Ella Barrett-Chan, MSI UBC
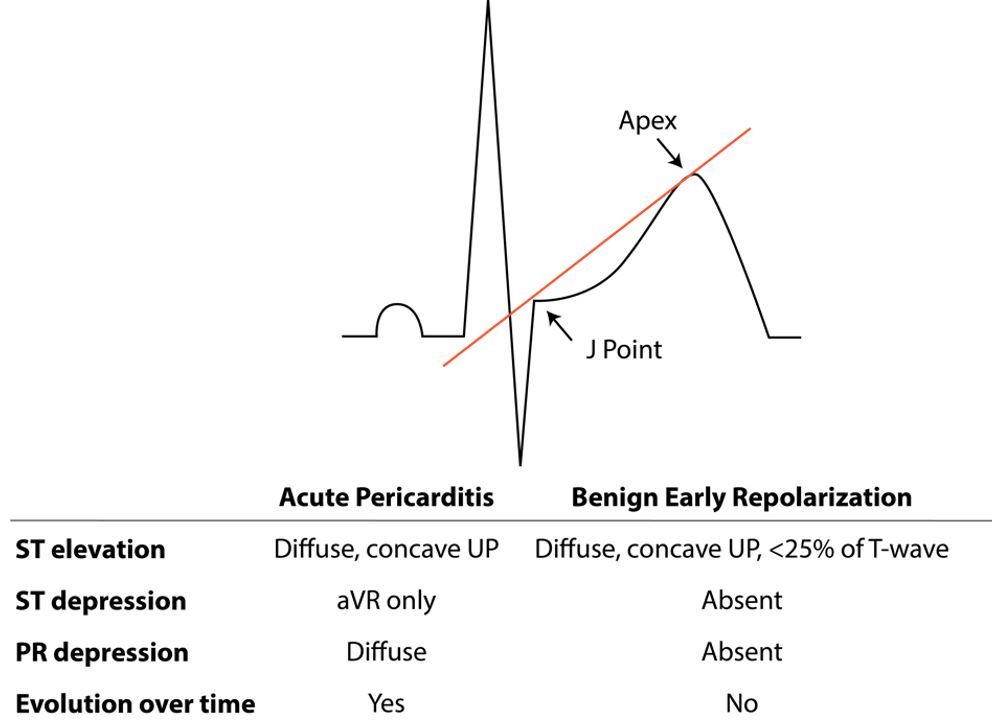
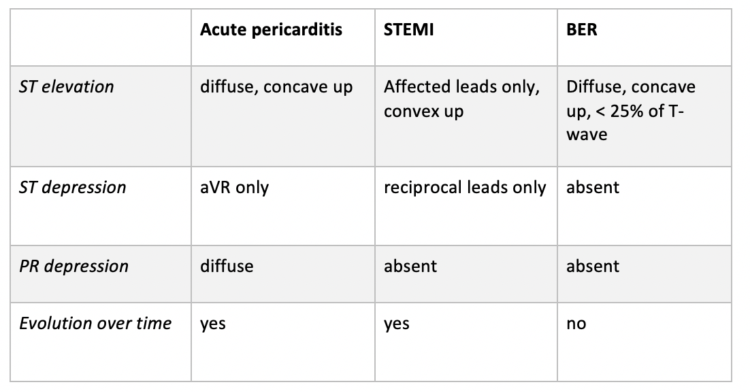
- Pericarditis features that differentiate it from ACS:
- ST elevation is ‘concave’ up but typically ‘convex’ up in ACS (figure 2)
- Down sloping T-P segments (“Spodick sign”)
- Absence of pathologic Q waves
- Absence of reciprocal ST changes
- Absence of QRS widening and QT prolongation in leads with ST elevation
Created By Ella Barrett-Chan, MSI UBC
- Differentiating pericarditis from benign early repolarization (BER)
- ST elevation is less than 25% of T-wave amplitude in BER
- ECG findings are stable over time in BER
- No PR depression in BER
Figure 3. Comparison of ECG changes in acute pericarditis, ST elevation MI and benign early repolarization.
Laboratory Findings
- WBC, CRP and ESR are likely to be elevated.
- Troponin may be elevated in 30% – concomitant myocarditis.
Imaging
- CXR typically normal
- Large pericardial effusion is uncommon – cardiomegaly.
- Transthoracic echocardiography
- Pericardial effusion in up to 60% of cases, often mild.
- Wall motion abnormalities suggest ACS rather than pericarditis.
Diagnostic Process
- Diagnosis of acute pericarditis requires at least two of the four main clinical criteria:
- Typical chest pain (> 85% cases).
- Pericardial friction rub (up to 30% cases).
- New widespread ST elevation or PR depression (up to 60% cases).
- Pericardial effusion (up to 60% cases).
- Supportive findings for diagnosis include: elevated inflammatory markers, evidence of pericardial inflammation through CT or CMR (not an ED issue).
- Diagnostic pericardiocentesis may be considered by cardiology, internal medicine.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Quality of evidence for the use of each diagnostic criteria is low and is based on the consensus of experts or small studies, retrospective studies or registries. The above diagnostic process has not been formally validated in a large scale study, however it remains widely agreed upon and stems from the 2015 European Society of Cardiology guidelines.
Related Information
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Cardiovascular EmergenciesRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jul 13, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.