Tension Pneumothorax
Cardinal Presentations / Presenting Problems, Critical Care / Resuscitation, Respiratory, Trauma
First 5 Minutes
Signs and Symptoms
- Respiratory Distress
- Vital Signs
- Hypoxia/requiring supplemental oxygen
- Tachypnea
- Tachycardia (50-75%)
- Hypotension (<25%)
- Exam
- Focused ultrasound shows pneumothorax.
- Absent ipsilateral breath sounds may be detected but sensitivity is only 50-75%.
- JVP distention and contralateral tracheal deviation important but poor sensitivity.
Treatment
- Decompression (needle or finger)
- Needle decompression – with 5-8 cm 10-14 gauge needle introduced at either
- 2nd anterior intercostal space, mid-clavicular line if thin chest wall.
- 4th/5th intercostal space, anterior-axillary line is now preferred.
- Finger thoracostomy
- 4th/5th intercostal space anterior-axillary line.
- Egress of air confirms diagnosis and temporarily relieves tension.
- Needle decompression – with 5-8 cm 10-14 gauge needle introduced at either
Context
- Life-threatening condition when rapidly progresses to hemodynamic collapse if not rapidly recognized and treated.
- Tension pneumothorax mechanism:
- Functional one-way valve at the site of pleural breech.
- Intrapleural air volume increases causing elevated intrapleural and intrathoracic pressures.
- Reduced venous return.
- Cardiac output is initially maintained via compensatory hyperpnea and tachycardia.
- When compensatory mechanisms fail (e.g., respiratory fatigue), are insufficient (e.g., very high intra-thoracic pressures) or are blunted (e.g., sedated mechanically ventilated patients) cardiac output drops precipitously resulting in hemodynamic collapse.
- Consider tension pneumothorax (ideally before cardiovascular instability and collapse):
- Chest trauma
- Chest pain
- Respiratory distress
- Hypoxemia
- Shock
- Cardiac arrest
- Post-intubation hypotension.
Diagnostic Process
- Primarily clinical findings and, time-permitting, imaging findings.
- Signs and Symptoms of tension pneumothorax include symptoms and signs of pneumothorax and (pending) cardiorespiratory compromise:
- History
- Pleuritic Chest pain – may radiate to ipsilateral back or shoulder.
- Respiratory distress
- Vital Signs
- Hypoxia/requiring supplemental oxygen
- Tachypnea
- Tachycardia (50-75%)
- Hypotension (<25%)
- Exam
- Respiratory distress
- Absent ipsilateral breath sounds (50-75% Sn)
- JVP distention (poor Sn, especially if concurrent hypovolemia
- Contralateral tracheal deviation (<25% Sn)
- Subcutaneous emphysema (high interobserver variability)
- Vital Signs
- Imaging
- Classically, tension pneumothorax is a clinical diagnosis.
- In suspected tension pneumothorax not in extremis (i.e., time permits), Point of Care US (POCUS) or X-ray improves diagnostic accuracy and avoids risks of unnecessary pleural decompression:
- Point-of-care ultrasound
- 94% Sn, 100% Sp for pneumothorax
- Features:
- Absent lung sliding (sensitive but not specific – other causes= , bullae, pleural adhesions).
- Absent comet tail artifact (not specific).
- Lung-point sign (transition point between normal and absent lung sliding, highly specific for pneumothorax).
-
- POCUS Identification of pneumothorax.
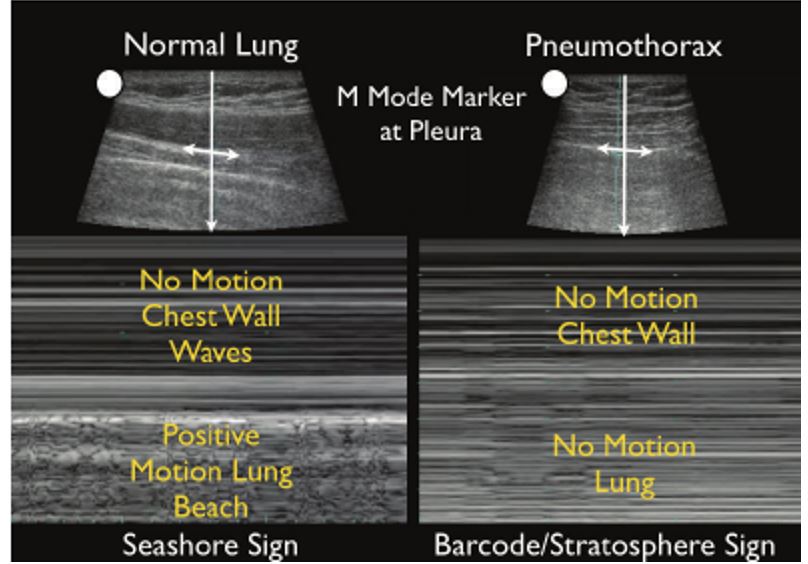
https://openi.nlm.nih.gov/detailedresult?img=PMC3485910_CCRP2012-503254.022&query=pneumothorax%20m%20mode&it=xg&req=4&npos=8 )
- Chest X-ray
- Pneumothorax:
- Visible lung edge.
- Absence of lung vasculature extending to thoracic wall.
- No X-ray findings are highly sensitive for tension pneumothorax:
- Ipsilateral increased intercostal spaces.
- Contralateral mediastinal shift (unreliable in adults due to low adult mediastinal compliance; in children have higher mediastinal compliance).
- Depression of the hemidiaphragm.
- Right sided Tension Pneumothorax on XR
- Pneumothorax:

https://openi.nlm.nih.gov/detailedresult?img=PMC4735541_KITP-12-26547-g003&query=tension%20pneumothorax&it=xg&req=4&npos=12
Recommended Treatment
ABC’s: Classic case where breathing (ptx decompression) takes precedence over airway and Circulation (B then A, C).
- Airway
- Breathing
- Decompression (needle or finger) and Aspiration
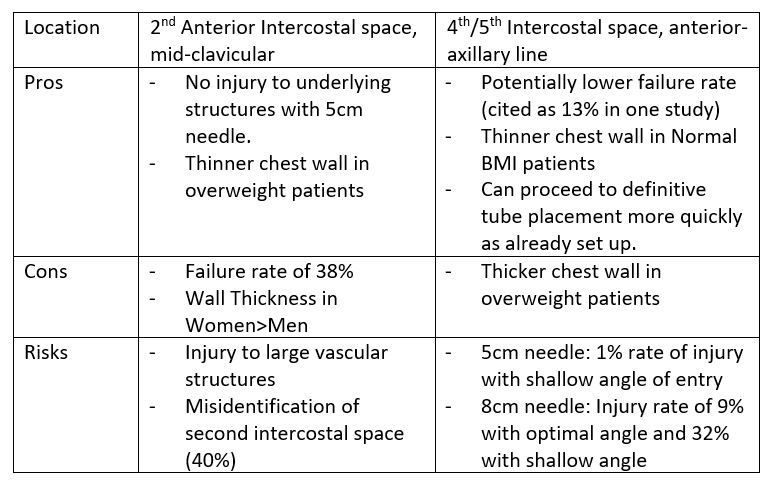
- Needle decompression – with 5-8cm 10 -14 gauge needle introduced at either
- 2nd anterior intercostal space, mid-clavicular line.
- 4th/5th intercostal space, anterior-axillary line (now preferred site).
- Needle decompression – with 5-8cm 10 -14 gauge needle introduced at either
- Decompression (needle or finger) and Aspiration
-
- Finger thoracostomy
- 4th/5th intercostal space along anterior-axillary line.
- Egress of air confirms diagnosis and temporarily relieves tension physiology.
- Catheter can be left in situ, however fails in 25% of cases due to kinking/dislodgement/occlusion therefore.
- Chest tube should be inserted immediately after decompression in all cases
- Spontaneous: Small bore 14F pigtail catheter.
- Traumatic: 28-32 French Chest tube.
- Chest tube pain may be managed by flushing tube with 10-20cc lidocaine or bupivacaine followed by NS; do not immediately reconnect to suction to avoid suctioning out anesthetic.
- Confirm placement with CXR.
- Disposition
- Tension Pneumothorax patients should generally be admitted to hospital for close observation and stabilization, especially if persistent air leak, bronchopleural fistula, concerns regarding patient reliability, or other concurrent indications for admission.
- Transfer to higher resource facility should be considered if local resources are insufficient.
- Reliable patients with small chest tube may be discharged from ED after 4-6hrs of observation post chest tube insertion, with means to return for reevaluation of chest tube.
- Upon CXR confirmation of lung re-expansion, chest tube can be removed.
- If there is an air leak present, discharge home with chest tube and repeat CXR q24h
- Upon CXR confirmation of lung re-expansion, chest tube can be removed.
- Tension Pneumothorax patients should generally be admitted to hospital for close observation and stabilization, especially if persistent air leak, bronchopleural fistula, concerns regarding patient reliability, or other concurrent indications for admission.
- Finger thoracostomy
Points to Consider
- Cardiac tamponade may mimic clinical features of tension pneumothorax (POC ultrasound to assess for this).
- Maintain high index of suspicion for tension pneumothorax in intubated patients.
- In stable patients, adequate analgesia with or without sedation should be administered to facilitate chest tube placement.
- Chest tubes may become plugged or mispositioned and cease to function. Do not assume patient with chest tube does not have tension pneumothorax if they are experiencing respiratory or hemodynamic instability.
- Patients should be educated to avoid air travel until complete resolution or for min 2 weeks after intervention (check with local expertise – Thoracic surgery or Respirology).
Criteria For Hospital Admission
- Admit all Tension Pneumothorax patients for observation and stabilization management until tension is resolved. Consider admission if persistent air leak, bronchopleural fistula, concerns regarding patient reliability or concurrent indications for admission.
Criteria For Transfer To Another Facility
- Following stabilization, if local resources are inadequate patient should be transferred/admitted at a trauma center equipped to manage Tension Pneumothorax and associated complications.
- For air transfers, extra care should be paid to ensuring chest tubes are functioning well and are well secured – low pressures may lead to worsening pneumothorax.
Criteria For Close Observation And/or Consult
Consult Thoracic Surgery for possible VATS bullectomy, pleurodesis if:
- Recurrent ipsilateral pneumothoraxes (2≤)
- Persistent air leak (≥3days)
- Extensive underlying lung disease
- High-risk occupation (ex. Pilots)
Criteria For Safe Discharge Home
Patient is hemodynamically stable after 4-6hrs of observation and:
- Improving on repeat CXR.
- Reliable to return for Chest tube follow-up.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Clinical features – High
- Clinical features consistent in various diagnostic guidelines.
US findings – HIGH
- Multiple studies show high sensitivity and specificity (≥90%) for pneumothorax detection with US.
Needle decompression – site, needle type/gauge.
- Study in Injury 2015 doesn’t support that 2nd intercostal space is thicker than 4th/5th intercostal space although most guidelines specify that 4/5th intercostal space should be used if first attempt at 2nd intercostal space is unsuccessful – either can be used.
- 4th/5th anterior axillary intercostal space has lowest predicted failure rate in multiple populations.
Related Information
OTHER RELEVANT INFORMATION
Needle Decompression Tutorial Video (spontaneous pneumothorax) – https://www.nejm.org/doi/full/10.1056/NEJMvcm1111468
POCUS Detection of Pneumothorax.
Reference List
Sharma A, Jindal P. Principles of diagnosis and management of traumatic pneumothorax. J Emerg Trauma Shock. 2008 Jan;1(1):34-41. doi: 10.4103/0974-2700.41789. PMID: 19561940; PMCID: PMC2700561.
Jalota Sahota R, Sayad E. Tension Pneumothorax. [Updated 2022 Nov 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559090/
MacDuffA, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax 2010;65:ii18-ii31.
Laan DV, Vu TD, Thiels CA, Pandian TK, Schiller HJ, Murad MH, Aho JM. Chest wall thickness and decompression failure: A systematic review and meta-analysis comparing anatomic locations in needle thoracostomy. Injury. 2016 Apr;47(4):797-804. doi: 10.1016/j.injury.2015.11.045. Epub 2015 Dec 13. PMID: 26724173; PMCID: PMC4976926.
Roberts DJ, Leigh-Smith S, Faris PD, et al. Clinical Presentation of Patients with Tension Pneumothorax. Annals of Surgery. 2015;261(6):1068-1078. doi:https://doi.org/10.1097/sla.0000000000001073
Seif D, Perera P, Mailhot T, Riley D, Mandavia D. Bedside Ultrasound in Resuscitation and the Rapid Ultrasound in Shock Protocol. Critical Care Research and Practice. 2012;2012:1-14. doi:https://doi.org/10.1155/2012/503254
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Dec 24, 2023
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.