The LRINEC Score for Suspected Necrotizing Soft Tissue Infections
Cardiovascular, Critical Care / Resuscitation
Context
Background:
- Necrotizing soft tissue infections (NSTIs), such as necrotizing fasciitis (NF), are rapidly progressive diseases associated with significant morbidity and mortality, and outcomes rely on prompt diagnosis, early initiation of antibiotics and surgical debridement.
- NSTIs can be difficult to diagnose early as their classic features of erythema, edema and pain out of proportion are relatively nonspecific and the more definitive visible signs, such as hemorrhagic bullae, crepitus, ecchymotic discoloration or superficial necrosis, are late manifestations.
The LRINEC Score:
- The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score was developed as a clinical decision tool to establish earlier NF diagnosis by helping distinguish it from other severe but non-necrotizing soft tissue infections, such as cellulitis or abscess.
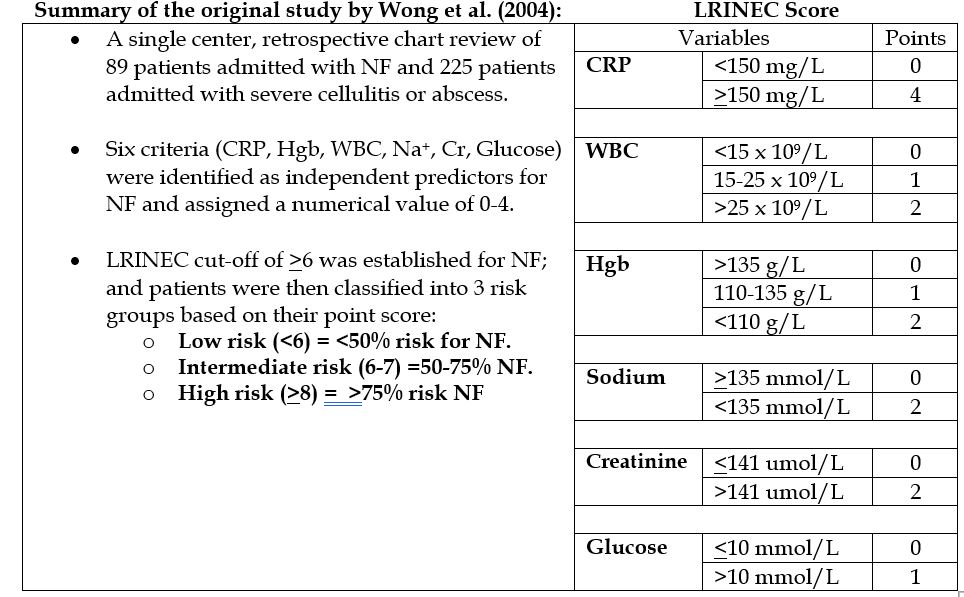
Pitfalls:
#1 – Poor sensitivity
- Recent meta-analytical data has shown significant variability in the LRINEC score’s sensitivity (ranging from 36% to 77%) which does not allow for clinicians to confidently identify and rule out NF.
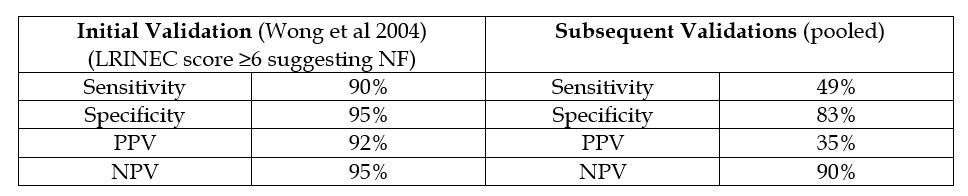
#2 – Poor external validation
- Subsequent trials attempting to validate the LRINEC score have failed to produce similar results. A summary comparing results is as follows:
#3 – Not validated in the ED
The original study used admitted patients and their admission bloodwork to derive their criteria. These were patients who could have therefore had more time to develop systemic derangement, and NOT who the ED clinician would be trying to screen for early disease.
#4 – Trying to detect early disease with late-stage markers
- The LRINEC score’s ability to differentiate it from other non-necrotizing infections is based on the ability to generate points, BUT it uses markers (WBC, HgB, sodium, creatinine and glucose) that elevate in response to severe systemic derangement to detect early disease. Therefore, it makes sense that early cases (which have not had time to develop systemic derangement) could go undetected.
Conclusions & Takeaways
- The LRINEC score may be used as an adjunct to assist with the clinical diagnosis. While it’s good specificity allows it to help differentiate NF from other non-necrotizing infections, its poor sensitivity and weak PPV render it a sub-optimal screening tool and incapable of confidently identifying early NF.
- Scores >6 are NOT diagnostic of NF.
- Scores of <6 DO NOT rule out NF.
- Recent literature has suggested that the LRINEC score’s strong NPV may have a future role as a rule out tool, but further studies are required.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Overall, the LRINEC score has been validated multiple times and shows promise diagnosing NF in certain populations, but the studies have been predominantly retrospective. Additional research with prospective and randomized controlled designs are still necessary to ensure adequate identification of NSTIs.
Related Information
Reference List
Hill J. Necrotizing Fasciitis and the Spectrum of Soft Tissue Infections. 2018. Available at: https://www.tamingthesru.com/blog/2018/9/3/necrotizing-fasciitis-and-the-spectrum-of-soft-tissue-infections. Accessed Dec 5, 2023.
Hwang C. LRINEC Score for Necrotizing Soft-Tissue Infection. 2018. Available at: https://www.ebmedicine.net/media_library/files/Calculated%20Decisions%20E0112%20LRINEC.pdf. Accessed Dec 5, 2023.
El-Menyar A, Asim M, Mudali IN, Mekkodathil A, Latifi R, Al-Thani H. The laboratory risk indicator for necrotizing fasciitis (LRINEC) scoring: the diagnostic and potential prognostic role. Scand J Trauma Resusc Emerg Med. 2017;25(1):28. Published 2017 Mar 7. doi:10.1186/s13049-017-0359-z
Wong CH, Khin LW, Heng KS, Tan KC, Low CO. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med. 2004;32(7):1535-1541. doi:10.1097/01.ccm.0000129486.35458.7d
April MD, Long B. What Is the Accuracy of Physical Examination, Imaging, and the LRINEC Score for the Diagnosis of Necrotizing Soft Tissue Infection?. Ann Emerg Med. 2019;73(1):22-24. doi:10.1016/j.annemergmed.2018.06.029
Kim DH, Kim SW, Hwang SH. Application of the laboratory risk indicator for necrotizing fasciitis score to the head and neck: a systematic review and meta-analysis. ANZ J Surg. 2022;92(7-8):1631-1637. doi:10.1111/ans.17459
Tarricone A, Mata K, Gee A, et al. A Systematic Review and Meta-Analysis of the Effectiveness of LRINEC Score for Predicting Upper and Lower Extremity Necrotizing Fasciitis. J Foot Ankle Surg. 2022;61(2):384-389. doi:10.1053/j.jfas.2021.09.015
Johnson LJ, Crisologo PA, Sivaganesan S, Caldwell CC, Henning J. Evaluation of the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score for detecting necrotizing soft tissue infections in patients with diabetes and lower extremity infection. Diabetes Res Clin Pract. 2021;171:108520. doi:10.1016/j.diabres.2020.108520
Bechar J, Sepehripour S, Hardwicke J, Filobbos G. Laboratory risk indicator for necrotising fasciitis (LRINEC) score for the assessment of early necrotising fasciitis: a systematic review of the literature. Ann R Coll Surg Engl. 2017 May;99(5):341-346. doi: 10.1308/rcsann.2017.0053. PMID: 28462647; PMCID: PMC5449710.
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 03, 2024
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.