Uncomplicated UTI/Cystitis – Management
Cardinal Presentations / Presenting Problems, Infections, Urological
Context
Uncomplicated UTI or Cystitis
- Typical symptoms: Dysuria, urinary frequency, urgency, suprapubic pain.
- No systemic symptoms (fevers, chills, nausea/vomiting), flank pain or CVA tenderness (see Complicated UTI – Management)
- Clinical diagnosis with typical symptoms: can use urinalysis to help with diagnosis when atypical symptoms.
- Urine Dipstick and Microscopy (see UTI (Adult) – Diagnosis)
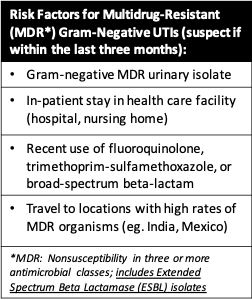
- Urine culture and sensitivity if risk factors for multi-drug resistant (MDR) gram negative organisms (see below).
- Microbiology:
- E. coli most common. Also Klebsiella, Proteus, S. saprophyticus.
- Consider MDR gram negative organism risk factors:
-
- Community-acquired ESBL E. coli risk factors include:
- Age > 60
- Diabetes mellitus
- Recurrent UTI
- Recent fluoroquinolones, cephalosporins (second or third generation), aminopenicillins
- Community-acquired ESBL E. coli risk factors include:
Recommended Treatment
Approach to Empiric Antibiotic Selection
Determine risk of infection with MDR gram-negative organism.
Low Risk of Resistance
- First-Line
- Nitrofurantoin (preferred)
- 100 mg PO BID x 5 days
- Avoid if suspecting early pyelonephritis or creatinine clearance < 30
- Trimethoprim-sulfamethoxazole (preferred)
- One double strength tab (160/800 mg) PO BID x 3 days
- If regional resistance rate > 20 % do not use
- Trimethoprim 100 mg BID x 3 days alternative equivalent
- Fosfomycin
- 3 grams of powder mixed in water, x 1 PO dose
- Susceptibility testing not routinely available.
- Avoid if suspecting early pyelonephritis.
- The above agents are equally effective. Considerations include:
- Allergies
- Expected adherence
- Local resistance patterns
- Recent use of one of the antibiotics in past 3 months. A different first-line antibiotic should be used if this criteria is met.
- Nitrofurantoin (preferred)
- Second-Line
- Beta-lactams
- Amoxicillin-clavulanate 500 mg BID x 5-7 d
- Cefadroxil 500 mg BID x 5-7 d (not first line)
- Do NOT use Ampicillin or Amoxicillin – high resistance rates.
- Fluoroquinolones
- Ciprofloxacin 250 mg q 12h x 3 d
- Ciprofloxacin 500 mg extended release q 24h x 3 d
- Levofloxacin 250 mg q 24h x 3 d
- Try to reserve for more severe infections
- Increasing resistance rates
- Beta-lactams
High Risk of Resistance
- First obtain urine culture and sensitivity.
- Empiric PO options:
- Nitrofurantoin (preferred)
- 100 mg BID x 5d
- Fosfomycin
- 3 grams of powder mixed in water, x 1 dose
- Nitrofurantoin (preferred)
- Note: Community Acquired ESBL
- Limited selection of PO antibiotics:
- Options include fosfomycin or nitrofurantoin. Amoxacillin-clavulanate may be an option, but use caution as there are reports of resistance.
- Resistance to ciprofloxacin, trimethoprim-sulfamethoxazole, and cephalosporins.
- Limited selection of PO antibiotics:
Considerations
- If unable to use empiric oral antibiotic options, can consider in healthy women with uncomplicated UTI to defer treatment until urine culture susceptibility results.
- If there is possible antibiotic resistance, but concerns for delaying treatment, it is reasonable to treat empirically with that antibiotic, while waiting for urine culture and susceptibility results.
- If concerned for treatment failure with PO antibiotics, treat with IV antibiotics (see Complicated UTI – Management)
- Symptomatic Treatment:
- Antibiotic therapy usually treats symptoms within 48 hours. Dysuria relieved as early as two hours.
- If severe dysuria, consider phenazopyridine, in addition to prescribed antibiotics.
- Urinary analgesic:
- Can use phenazopyridine 200 mg TID PRN x 2d
- Do not use chronically, as can mask UTI symptoms.
- Can cause methemoglobinemia.
Additional Considerations
- Use regional/institutional antibiogram (in BC, use Spectrum App) to help with empiric antibiotic selection.
- However, use urine culture and sensitivity to guide treatment, if taken based on above indications (generally not required in Uncomplicated UTI/Cystitis).
Disposition / Follow-Up
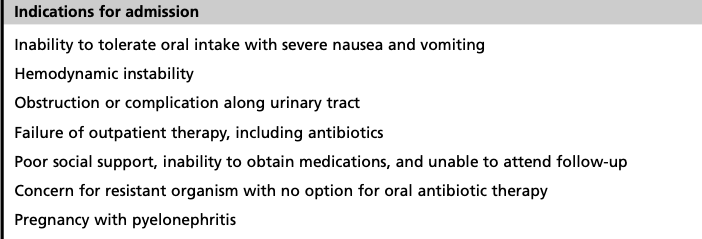
Uncomplicated UTI/Cystitis are rarely admitted
Indications to consider admission include
Follow-up
- Patients prescribed antibiotics should have healthcare follow-up for resolution of symptoms.
- Note: if hematuria on initial presentation, repeat urinalysis in approximately 6 weeks following completion of antibiotics to evaluate for persistent hematuria.
- Urine culture and susceptibility should be followed up to ensure appropriate antibiotics.
- Patients that do not improve after 1-2 days of antibiotics should return to ED for further workup:
- UTI mimic?
- Complicated UTI?
- Perform urine culture and sensitivity, if not done already.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The above summary is taken from recent literature reviews on emergency department diagnosis and management of UTIs.
Related Information
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jun 18, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.