Difficult Airway Management
Critical Care / Resuscitation, Respiratory
Context
Resuscitative airway management in the emergency department (ED) is inherently difficult by definition, and the practitioner should always be prepared for a difficult airway especially given the relatively poor test characteristics regarding difficult airway predictive tools.
Management
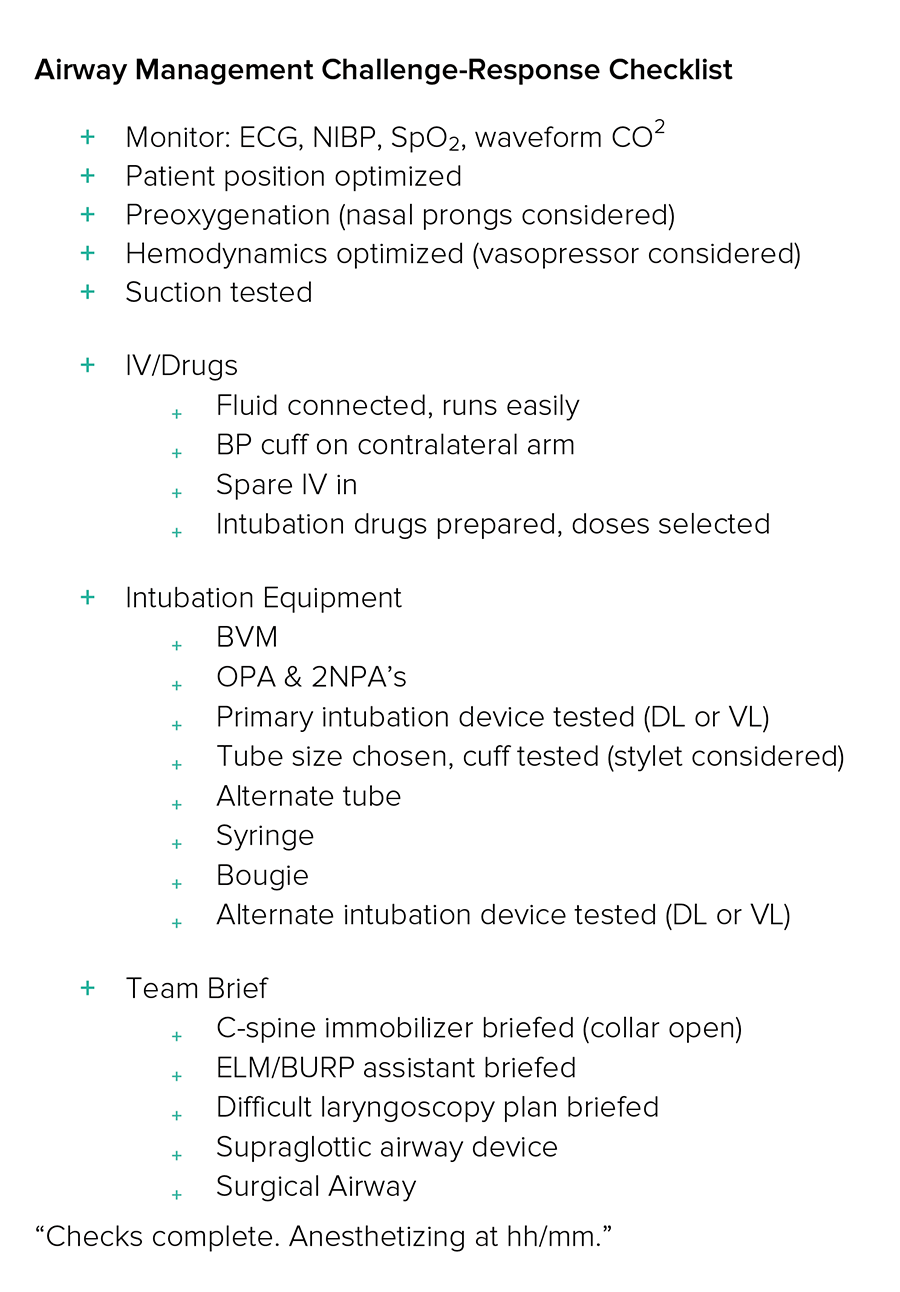
- Preparation for a difficult airway should include:
- Careful consideration of pharmacology in relation to RSI and consideration of awake intubation if there are no contraindications including an uncooperative patient or altered level of consciousness.
- An extraglottic device should be ready for use.
- A bougie should be open and directly accessible.
- An alternative intubation device (video or direct laryngoscopy) should be prepared;
- A call for assistance should be made;
- Optimization of oxygenation should be performed using Bag Mask Ventilation (BMV) or positive pressure device and high flow nasal prongs.
- The neck should be palpated and marked in preparation and prediction of possible surgical airway intervention and
- All associated tools (primary, supraglottic, surgical) should be ready and open.
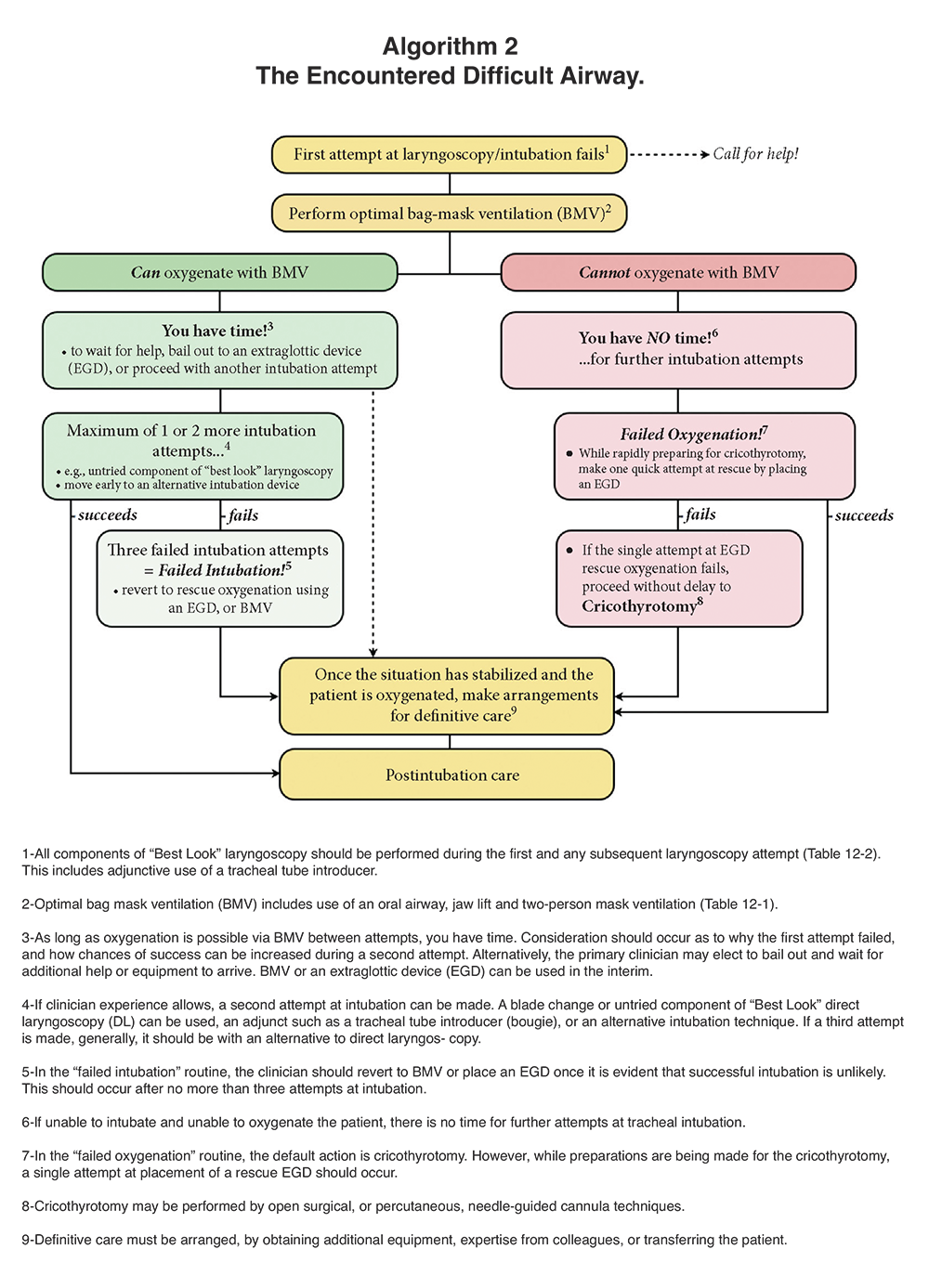
- Once encountered a firm plan and interventions with the resuscitation team engaged (however large or small) must be performed. See below algorithm “The Encountered Difficult Airway”.
- Optimization of BMV starts with patient positioning (if not contraindicated), confirmation of oxygenation source and use of high flow nasal prongs conjointly (for at least 3 minutes if time allows).
- BMV is best performed using oral airway, nasal trumpets, two-person technique, obviation of oral/pharyngeal foreign body and jaw thrust in conjunction with early use of a supraglottic device.
- Second and third attempts at laryngoscopy must include optimization and augmentation/change in technique including use of bougie, external laryngeal manipulation, use of Direct Laryngoscopy or Video Laryngoscopy and intubation by the most experienced airway practitioner.
- If cricoid pressure had been used in the context of a rapid sequence intubation (RSI) then it should be discontinued.
Challenge-Response Checklist
Difficult Airway Algorithm
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Expert consensus as per 2015 Difficult Airway Society Guidelines.
Reference: Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. C. Frerk, V. S. Mitchell, A. F. McNarry, C. Mendonca, R. Bhagrath, A. Patel, E. P. O’Sullivan, N. M. Woodall and I. Ahmad, Difficult Airway Society intubation guidelines working group British Journal of Anaesthesia, 115 (6): 827–848 (2015) doi:10.1093/bja/aev371.
Related Information
OTHER RELEVANT INFORMATION
Difficult Airway Society Guidelines – accessed July 25, 2017.
AIME Airway Interventions and Management in Emergencies – accessed July 25, 2017.
The above image of Difficult Airway Algorithm is used with permission. Source:
Airway Management in Emergencies – Open-access online textbook from www.aimeairway.ca.
Reference List
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Oct 30, 2018
Visit our website at https://emergencycarebc.ca
COMMENTS (1)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.