Pericarditis – Treatment
Cardiovascular, Inflammatory
Context
- True incidence of pericarditis unknown: 5% of non-ACS “chest pain” ED visits.
- Cardiac tamponade can occur in up to 15% of cases.
- Important to distinguish from ACS.
- Inflammatory condition of the pericardium:
- Infectious etiologies
- Most common cause is viral or idiopathic as etiologic agent is rarely identified.
- Consider tuberculosis if recent travel to an endemic region.
- Non-infectious etiologies
- Autoimmune conditions – SLE, RA, scleroderma, sarcoid, vasculitis.
- Autoinflammatory pericardial syndromes (Dressler syndrome): post myocardial infarction, cardiac surgery or cardiac trauma.
- Neoplastic: (metastatic: lung>breast>leukaemia and lymphoma>melanoma).
- Radiation.
- Metabolic (uremia).
- Drug-related.
- Symptoms usually last 4-6 weeks but other forms exist
- Incessant pericarditis: up to 3 months.
- Recurrent/relapsing pericarditis: symptoms recur after a symptom-free period.
- Chronic pericarditis: symptoms > 3 months.
- Infectious etiologies
Disposition
- Outpatient management is recommended for low-risk patients who have no criteria for hospital admission.
- Consider admission/same-day consult:
- For diagnosis or etiologic ambiguity: Underlying etiology unlikely to be viral/idiopathic.
- Myocarditis or myopericarditis (significant troponin elevation).
- Significant abnormal vital signs or tachycardia out of proportion to pain/fever.
- Large pericardial effusion (> 20 mm on echo).
- Relapsing/recurrent, incessant or chronic pericarditis.
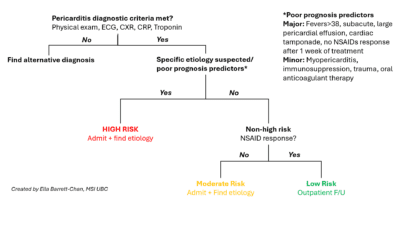
- Figure 2 below outlines triage scheme of pericarditis.
Click to enlarge the diagram
Recommended Treatment of Acute Pericarditis
- Restrict physical activity (minimal activity) until resolution of symptoms and normalization of CRP.
- Treat underlying condition (ex. Antibiotics for purulent pericarditis).
- First line treatment
- NSAIDs OR Aspirin + Colchicine.
- Recommend GI protection with PPI.
- Second line treatment
- Prednisone + Colchicine.
- In retrospective studies steroids associated with higher recurrence rate.
- Only use steroids if contraindications to NSAIDs/Aspirin or specific indication (ex. systemic inflammatory disease).
- Prednisone + Colchicine.
Dosing
- NSAIDs
- Ibuprofen 600-800 mg po q8h.
- 7-14 days, then taper by 200-400 mg every 1-2 weeks.
- Aspirin 750 to 1000 mg po TID in patients with concomitant CAD.
- 7-14 days, then taper by 250-500 mg every 1-2 weeks.
- Ibuprofen 600-800 mg po q8h.
- Colchicine
- Patients > 70 kg: 0.5 mg PO BID.
- Patients < 70 kg: 0.5 mg PO daily.
- Duration: 3 months.
- Tapering not required.
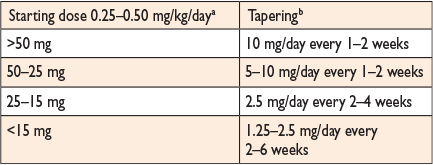
- Prednisone
- 0.2-0.5 mg/kg/day PO.
- Slow taper recommended (see table in Figure 1).
- Requires exclusion of infectious (bacteria / TB) etiology.
Figure 2: Recommended tapering schedule of prednisone based on starting dose.
Source: Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. Eur Heart J. 2015;36(42):2921-2964. doi:10.1093/eurheartj/ehv318
Procedural/Surgical
- If there is high clinical suspicion for cardiac tamponade, drainage of the pericardial fluid is required urgently.
- Needle pericardiocentesis with FAST US, echocardiographic or fluoroscopic guidance.
- Surgical drainage.
- See emergent pericardiocentesis video: Emergency Pericardiocentesis.
Criteria For Transfer To Another Facility
- Site/region specific.
- Consider hemodynamic stability and length of travel prior to transport.
Criteria For Safe Discharge Home
- Follow up with primary care provider (unless consultant involved) within 7 days to ensure adequate response to treatment and monitoring of CRP.
Prognosis
- Prognosis for acute viral/idiopathic pericarditis is quite good with treatment.
- Cardiac tamponade rarely occurs.
- Constrictive pericarditis develops in less than 1%.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Recommendation for Aspirin or NSAID + Colchicine for first line treatment of acute pericarditis.
Recommendation for outpatient management for low risk patients and hospital admission for high risk patients with at least one risk factor.
Use of CRP and resolution of symptoms to guide return to physical activity.
Related Information
Reference List
Relevant Resources
RELEVANT RESEARCH IN BC
Cardiovascular EmergenciesRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jul 13, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (2)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.