Pulmonary Embolism – Diagnosis
Cardiovascular, Hematological / Oncological, Respiratory
Context
- Pulmonary embolism (PE) is a major cause of morbidity and mortality worldwide and requires timely diagnosis and treatment.
- In Canada, the incidence rate of PE is 0.38 per 1000 person years
- Higher risk patients include those with active cancer, age >80, pregnancy, trauma, recent surgery, immobility, genetic predisposition or past VTE
- Up to 50% are unprovoked2
- The clinical starting point for the diagnosis of PE in suspected patients is to estimate the likelihood based on clinical features. Presentations are variable so keeping suspicion initially high is important.
- The most common presenting complaints of patients with PE are dyspnea and pleuritic chest pain. Other clinical findings may include: cough, substernal chest pain, fever, hemoptysis, syncope, signs of DVT.4
- Diagnostic test findings that may suggest PE:
- ECG – sinus tach, signs of right heart strain (S1Q3T3, T wave inversions V1-3, RBBB)
- CXR – Westermark sign (focal area of translucency due to oligemia) or Hampton’s hump (wedge-shaped opacity with a rounded convex apex toward the hilum)
- Point-of-Care Ultrasound – RV strain (RV dilation, septal flattening). McConnell sign is said to be specific but not sensitive (Video: Right Heart Strain)
- Lab – elevated Troponin and/or BNP
- These findings are often not found in stable patients with small to moderate sized PE.
Diagnostic Process for Stable Patients
- Choosing Wisely Canada guidelines recommend risk stratification using a clinical decision rule prior to ordering a CT Pulmonary Angiogram (CTPA) or Ventilation/Perfusion (VQ) scan in patients with suspected PE. In general, if a pretest probability (PTP) is <2.5% for a disease, there is likely to be more harm than benefit for diagnostic imaging tests.
- The first step in selecting a diagnostic approach is to develop a PTP for PE.
- Patients with a lower PTP (<15%) stratified by the application of the Well’s criteria for PE, should be further risk stratified using the Pulmonary Embolus Rule Out Criteria (PERC) rule or with the use of a D-dimer test.5
- A negative PERC score means that the likelihood of PE is < 2%.
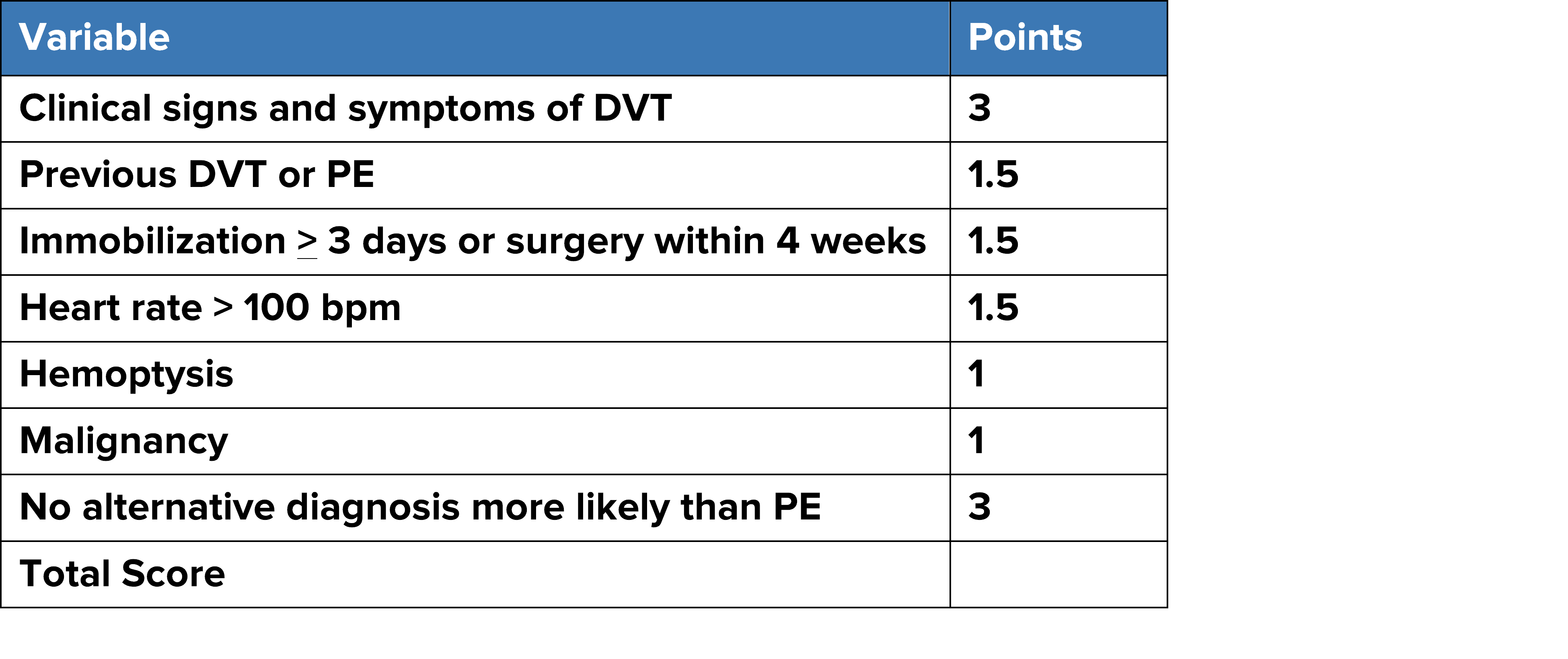
STEP 1: Apply the Well’s Score for PE (MDCalc to calculate Wells score)
**Wells Total Score: >4.5 PE is likely. Arrange for imaging. Anticoagulate if no contraindications and delay more than 4 hours.
**Wells Total Score: <4.5 PE is unlikely (< 15%). Apply PERC rule.
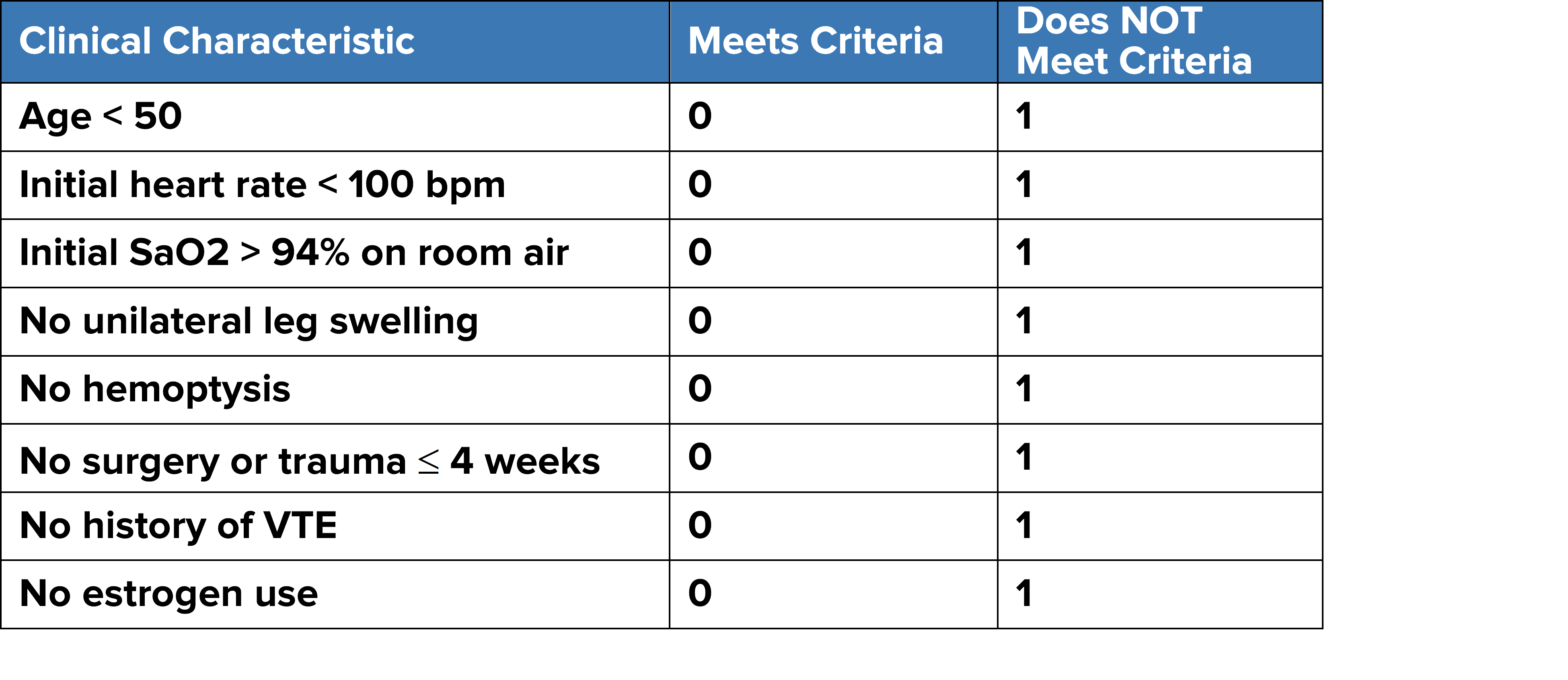
STEP 2: Apply PERC Rule (MDCalc to calculate PERC rule)
- If PERC negative (Score=0): STOP. Chance of PE is < 2%.
- If ANY PERC point is positive, PE cannot be excluded.
STEP 3: Order a D-dimer
- If D-dimer negative: STOP.
- apply age-adjusted D-dimer criteria for those age > 50yrs11
- Formula: age (in years) x 10 mcg/L
- For example, if your patient is 70 years of age, their cutoff D-dimer score will be 700 mcg/L (70 x 10 mcg/L).
*Note: be sure to check the units of your hospitals D-dimer assay
- If D-dimer positive: Arrange for imaging. Anticoagulate if no contraindications and imaging is delayed more than 4 hours.
Diagnostic Imaging
- CTPA – this is the imaging modality of choice in most patients.
- VQ scan – for patients with renal insufficiency contrast allergy, young patients and pregnant women.
- Consult radiology if there is any question about the optimal imaging modality. Risk of worsening renal failure is not as high as once thought.
Unstable Patients
- Determine the cause for shock (Clinical Summary coming soon to BC EMN) and manage accordingly.
- If there is a high probability for PE based on clinical features then start empiric treatment urgently and order confirmatory testing.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
The components of this diagnostic strategy have been carefully developed and validated.
Related Information
Reference List
Thrombosis Canada. Clinical Guides 2018. From: http://thrombosiscanada.ca/wp-content/uploads/2018/04/Pulmonary-Embolism-Diagnosis-2018Apr03.pdf
-
Choosing Wisely Canada Recommendations 2018. Retrieved September 2018 from: https://choosingwiselycanada.org/emergency-medicine/
-
-
-
-
Pulmonary Embolism. Susan R. Kahn,M.D., and Kerstin de Wit, M.B., Ch.B.,M.D.
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Sep 06, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.