Pulmonary Embolism – Treatment
Cardiovascular, Hematological / Oncological, Respiratory
Context
Venous thromboembolism (VTE), including deep vein thrombosis and pulmonary embolism (PE), is common, affecting 1-2/1000 adults per year.
Up to 10% of symptomatic PE result in death within 1 hour of symptom onset. Early diagnosis and treatment reduce morbidity and mortality for the rest.
Supportive Therapy
Administer O2 to keep SaO2 > 90%, including high-flow O2, or mechanical ventilation if indicated (i.e. cardiac arrest)1.
Context
Thrombosis Canada – PE Treatment Guidelines (https://thrombosiscanada.ca/clinicalguides/# ).
- High pre-test probability (PTP) (Wells Score ≥ 6) – promptly initiate anticoagulation, unless bleeding risk is high.
- Intermediate PTP (Wells Score 2 – 5.5) – treatment can be withheld if diagnostic imaging within 4 hours.
- Low PTP (Wells Score ≤ 1.5) – treatment can be withheld if diagnostic imaging within 24 hours2.
Wells’ Criteria for Pulmonary Embolism / PE (https://thrombosiscanada.ca/tools/?calc=wellsPE ).
|
Points |
|
|
Clinical Signs and Symptoms of DVT |
3 |
|
PE Is #1 Diagnosis, or Equally Likely |
3 |
|
Heart Rate > 100 |
1.5 |
|
Immobilization at least 3 days, or Surgery in the previous 4 weeks |
1.5 |
|
Previous, objectively diagnosed PE or DVT |
1.5 |
|
Hemoptysis |
1 |
|
Malignancy w/ Treatment within 6 mo, or palliative |
1 |
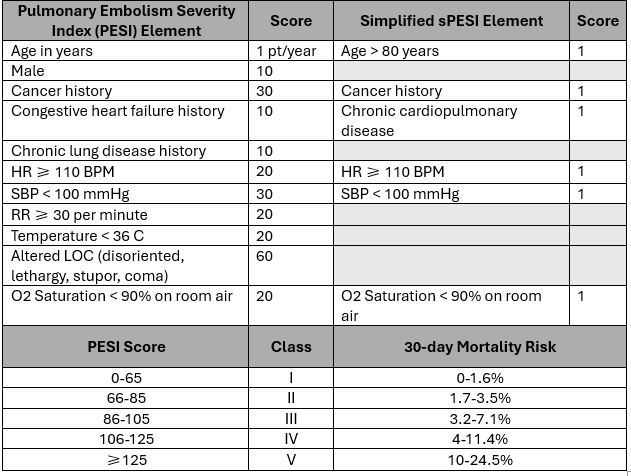
Stratify to inpatient vs outpatient management using Pulmonary Embolism Severity Index (PESI) or simplified PESI (sPESI).
MD CALC: https://www.mdcalc.com/pulmonary-embolism-severity-index-pesi
Thrombosis :
- PESI: https://thrombosiscanada.ca/tools/?calc=pesi
- sPESI: https://thrombosiscanada.ca/tools/?calc=simplifiedPesi
Consider outpatient management for very low- or low-risk patients:
- PESI = Class I or II OR sPESI = 0 ,
- Approximately half of the cases in emergency departments classified in this category,
- Consider individual patient factors:
- oxygen need, pain control, bleeding risk, renal dysfunction, social support2.
Classification:
Massive PE: Presence of shock or persistent hypotension (systolic BP <90 mmHg, or drop in systolic BP of ≥40 mmHg), for over 15 minutes, if not caused by new onset arrhythmia, hypovolemia or sepsis.
- Accounts for 5% of PE cases, short-term mortality >15%.
Non-massive PE: Hemodynamically stable patients. Don’t meet criteria for massive PE4.
Anticoagulation
If thrombolysis required, IV unfractionated heparin (UFH) preferred. Otherwise, choice of anticoagulant should not depend on severity of PE or clot burden2.
Anticoagulation should be continued for a minimum of 3 months, after which risk/benefits of treatment should be re-assessed1,2.
Options available:
- DOAC monotherapy (apixaban/rivaroxaban).
- DOAC (dabigatran/edoxaban) therapy, with initial bridging UFH or LMWH.
- Warfarin therapy, with initial bridging UFH or LMWH.
- LMWH monotherapy.
Generally, DOACs are preferred over warfarin (lower risk of bleeding), unless contraindications.
Apixaban: 10 mg BID for 7 days, followed by 5 mg BID. Use with caution for CrCl 15-29 mL/min. Not recommended with CrCl <15 mL/in, or in patients undergoing dialysis.
Rivaroxaban: 15 mg BID for 21 days, followed by 20 mg QD. Use with caution for CrCl 15-30 mL/min. Not recommended with CrCl <15 mL/in.
Dabigatran: Begin with 5-10 days LMWH. Then give dabigatran 150 mg BID. If ≥80 years of age, or high risk of bleeding, dose may be lowered to 110 mg BID. Contraindicated with CrCl <30 mL/min.
Edoxaban: Begin with 5-10 days LMWH. Then give edoxaban 60 mg BID. Lower dose to 30 mg BID for body weight ≤60 kg, CrCl 30-50 mL/min, or concurrent PGP inhibitor use (except amiodarone and verapamil). Not recommended with CrCl <30 mL/min2.
*DOACs should not be used in pregnant/breastfeeding women, or patients with significant renal or hepatic dysfunction.
UFH carries higher risk overall but benefit > risk for:
- Patients with severe renal insufficiency (CrCl < 30 mL/min).
- Patients at very high risk for bleeding, and who may require rapid reversal of anticoagulant.
- Patients who receive thrombolytic therapy2.
Thrombolysis
Systemic Thrombolysis.
Thrombolysis is generally only indicated for massive PE.
If patient has submassive PE, with persistent signs/symptoms of right heart failure or cardiopulmonary deterioration: consult hematologist/internal medicine.
Thrombolytic therapy can be completed with recombinant tPA (rt-PA), OR tenecteplase.
Dosing options include:
- Recombinant tPA – various options to choose from:
- 100 mg over 2 hours1.
OR
- 6 mg/kg (max 50 mg) over 15 minutes.
OR
- 5 mg/kg (max 50 mg): 10 mg bolus, remainder over 2 hours.
European Society of Cardiology recommends 100 mg over 2 hours1.
2. Tenectaplase dose of 30-50 mg: bolus over 5-10 seconds.
In patients with cardiac arrest: rt-PA dose of 50 mg: bolus over 1 minute2.
Intravenous UFH (without a bolus) should be used initially after thrombolytic therapy, followed by a transition to a longer-term agent.
Catheter-directed thrombolysis
Considered with massive PE in consultation with a specialist in multidisciplinary setting2,5. Lower risk of bleeding compared to systemic thrombolytic therapy2,5.
Generally used in:
- Hemodynamic instability with failed systemic thrombolysis.
- Hemodynamic stability + right ventricular dysfunction with failed anticoagulation.
- High risk of bleeding with systemic thrombolysis6.
If thrombolysis is contraindicated, surgical embolectomy may be considered7.
Patients with contraindication for anticoagulation.
IVC filters may be used when anticoagulation is absolutely contraindicated. Retrievable filters are recommended and should be removed as soon as possible.
Routine use not recommended – high rate of complications, including increased risk of DVT.
Cancer
Weight-adjusted LMWH should be considered for the first 6 months.
Edoxaban or rivaroxaban indicated if:
- Active non-GI cancer.
- Not high risk for GI bleed.
- No drug-drug interactions.
Edoxaban: Initiate minimum 5 days on LMWH. Then edoxaban 60 mg QD. Reduce to 30 mg QD with CrCl 30-50 mL/min, weight ≤ 60 kg or concurrent PGP inhibitor use.
Rivaroxaban: Follow same dosing as the non-cancer population.
Edoxaban is preferred over rivaroxaban for this population1.
Patients should receive therapy for 3-6 months, and may be extended if:
- Concurrent systemic chemotherapy.
- Metastatic disease.
- Progressive/relapsed disease.
- Other prothrombotic risk factors2.
Pregnancy
LMWH or UFH are safe during pregnancy. LMWH is the drug of choice unless:
- Patient has heparin induced thrombocytopenia (HIT) /history of HIT.
- Severe renal dysfunction.
Anticoagulation should be continued for a minimum of 3 months. Often continued until at least 6 weeks postpartum due to increased risk of VTE in pregnancy2.
Warfarin is contraindicated in pregnancy, okay during breastfeeding.
DOACs should be avoided in pregnancy and breastfeeding1,2.
Criteria For Hospital Admission
Disposition
Patients with massive PE, or those receiving thrombolytic treatment are generally placed in the ICU. Patients deemed to be low-risk and are able to adhere to treatment are generally treated as outpatients and are discharged.
Indications for admission:
- PESI Class ≥ 3, sPESI ≥ 1
- Alternatively, ≥ 1 Hestia criterion.
2.Risk of non-compliance, or loss to follow-up.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Use of DOACs over warfarin for treatment of VTE: High: Systematic review and meta-analysis comparing DOACs to warfarin: DOACs demonstrate non-inferiority as well as significant reduction in intracranial bleeding and fatal bleeding8.
Thrombolytic therapy in massive PE: High: Thrombolytic therapy significantly reduced all-cause mortality in massive PE, but was not significant in hemodynamically stable patients9,10.
Catheter-directed thrombolysis (CDT): Low: Lack of studies directly comparing CDT to systemic thrombolysis1.
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jul 10, 2020
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.