Systemic Lupus Erythematosus (SLE)
Cardiovascular, Ears, Eyes, Nose, and Throat, Gastrointestinal, Infections, Neurological, Respiratory
Context
Chronic autoimmune disease of unknown, multifactorial etiology. It presents a challenge to emergency providers due to its diverse and sometimes life-threatening manifestations.
Affects between 20-70 per 100,000 individuals, with 90% of the cases in women, and a higher prevalence in Asian, African American, African Caribbean, and Hispanic American individuals compared with White individuals.
Can cause manifestations in virtually any organ system through inappropriate immune response to self.
Diagnostic Process
Clinical Manifestations:
|
Common Presentations |
Emergent Conditions |
|
|
Neuropsychiatric |
Psychosis, mood disorders, peripheral neuropathy, headache |
Seizure, stroke, sinus thrombosis, CNS vasculitis, transverse myelitis, spinal artery thrombosis, lupus psychosis |
|
Cardiologic |
Pericarditis, valvular abnormalities |
Pericardial effusion, cardiac tamponade, acute coronary syndrome, Libman-Sacks endocarditis |
|
Pulmonary |
Pleuritis, interstitial lung disease, pulmonary hypertension |
Pulmonary embolism, pneumonia, acute lupus pneumonitis, alveolar hemorrhage |
|
Gastrointestinal |
Intestinal pseudo-obstruction |
Acute abdominal pain, mesenteric vasculitis |
|
Dermatologic |
Malar rash, discoid lupus, oral/nasal ulceration |
Systemic vasculitis, digital gangrene |
|
Musculoskeletal |
Polyarthralgias, polymyalgias, avascular necrosis |
Septic arthritis |
|
Hematological |
Mild-moderate anemia/leukopenia/thrombocytopenia, antiphospholipid syndrome (APS) |
Severe thrombocytopenia/APS, acute hemolytic anemia |
|
Renal |
CKD |
Lupus nephritis |
- Potential constitutional manifestations of SLE include fever, fatigue, weight loss. Infections are also a potential emergent complication of SLE, and providers should rule out opportunistic infections if the patient is immunocompromised, and sepsis depending on the clinical context.
- Up to 40% of SLE patients may also present with manifestations of antiphospholipid syndrome (APS), which range from sequelae of thrombosis and thromboembolism to catastrophic APS, which presents with multiple thrombotic sites and organ failure.
Physical Examination:
- A complete and thorough examination in those who you suspect a diagnosis of SLE to be present is warranted.
Investigations:
- CBC, urinalysis, creatinine, should be routinely obtained to assess for signs of increased disease activity or systemic inflammatory process.
- In patients with suspected SLE, ANA, anti-dsDNA, anti-Smith antibody, antiphospholipid antibodies (lupus anticoagulant, IgG/IgM anticardiolipin antibodies, IgG/IgM anti-beta2-glycoprotein 1), C3/C4, ESR/CRP, and urine protein to creatinine ratios should be obtained. These can be ordered with outpatient follow-up organized for evaluation of the results.
- In patients with known SLE and chest pain, ACS should be ruled out and cardiac workup is warranted including ECG, stress test and troponin.
- Diagnostic imaging is not routinely obtained but can be valuable based on the symptoms.
Diagnostic Considerations:
- In the emergency department (ED), care providers will often see patients with SLE presenting with an exacerbation or complications from the disease or their medications.
- However, patients with suspected, but no formal diagnosis of SLE may present to the ED.
- Formally, a diagnosis is made using the 1997 ACR criteria or the 2012 SLICC criteria, but diagnosis in the ED is difficult to make given the broad manifestations of the disease and the time it takes for laboratory results to return.
- A number of other diseases are often mistaken for SLE prior to diagnosis, including undifferentiated connective tissue disease, primary Sjögren’s syndrome, primary APS, fibromyalgia with positive antinuclear antibody, idiopathic thrombocytopenic purpura, drug-induced lupus, and early rheumatoid arthritis.
Many medications are known to cause lupus-like autoimmune response and may be mistaken for SLE (see table below):
|
Drugs associated with lupus-like autoimmune responses |
|||
|
Drug |
High risk (>5%) |
Moderate risk (1-5%) |
Low risk (0.1-1%) |
|
Procainamide, hydralazine |
Quinidine |
Penicillamine, carbamazepine, methyldopa, sulfasalazine, minocycline, chlorpromazine, propylthiouracil, isoniazid |
|
Recommended Treatment
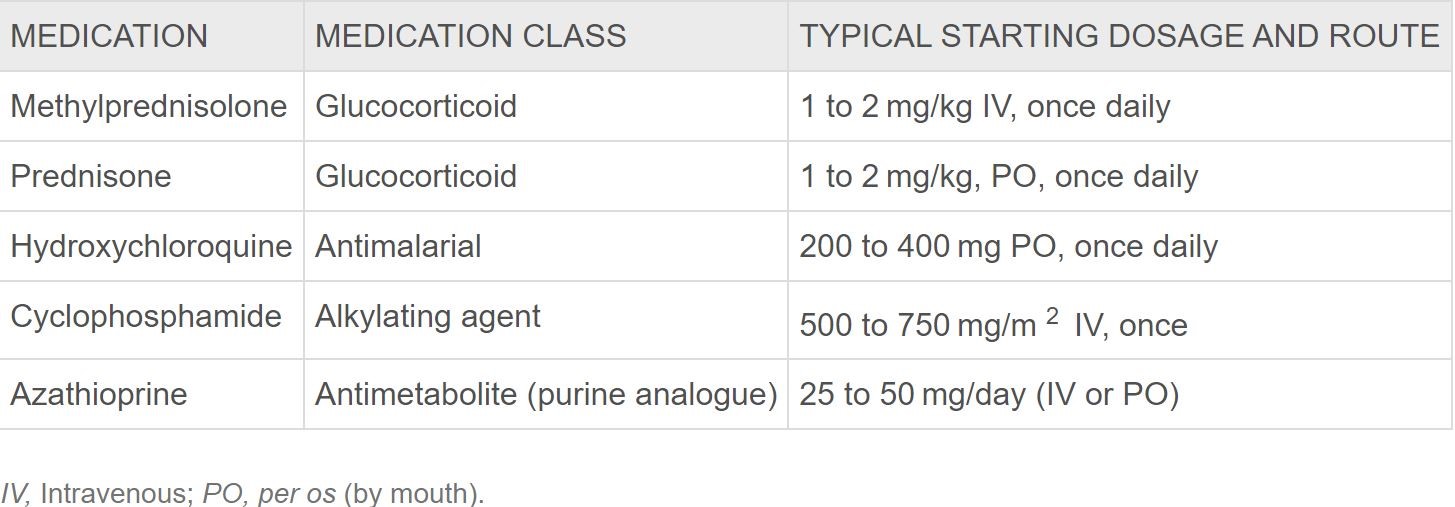
- For non-infectious consequences of SLE, introduction or modulation of immunomodulating therapy is warranted.
Image from Rosen’s Emergency Medicine 9th Edition
- For infections in SLE patients who are on chronic steroid therapy, a stress dose of glucocorticoids (i.e. hydrocortisone 50-100 mg IV every 8 hours) + appropriate antimicrobial coverage should be initiated.
- Many symptoms related to SLE are related to inflammation and are amenable to NSAIDs. In patients with CKD or peptic ulcer disease, where NSAIDs are contraindicated, alternatives include acetaminophen and narcotics.
- For drug-induced lupus, cessation of the offending agent is therapeutic, and NSAIDs/steroids can be used for symptom control.
- For acute thrombotic events, unfractionated or low-molecular-weight heparin is indicated. In catastrophic APS, in addition to glucocorticoids and anticoagulation, IVIG, plasma exchange, and cyclophosphamide can be considered.
Criteria For Safe Discharge Home
- Non-life-threatening presentation.
- Appropriate follow-up as an outpatient is available.
- If the patient had undifferentiated chest pain with ACS ruled out in the ED, they should have expedited evaluation with a stress test in an observation unit or outpatient basis. If stress test is done in an outpatient setting, daily aspirin should be prescribed.
Criteria For Hospital Admission
- Presentation of SLE flare, new thrombotic events, infection, or life-threatening presentation.
Criteria for ICU admission:
- Progressive circulatory or respiratory derangement in spite of initial resuscitation.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Diagnosis of SLE using the 1997 ACR and 2012 SLICC criteria have high sensitivity and specificity – HIGH
Related Information
Reference List
Systemic Lupus Erythematosus and the Vasculitides. In Rosen’s emergency medicine: concepts and clinical practice. Arntfield, R.T. & Hicks, C.M. (2018). (9th ed., 1402-1417).
– Elsevier.Clinical manifestations and diagnosis of systemic lupus erythematosus in adults.
Wallace, D.J. & Gladman, D.D. (2021).Retrieved December 14, 2021-UpToDate
Drug-induced lupus.
Merola, J.F. (2021). Retrieved December 15, 2021
-UpToDateEpidemiology and pathogenesis of systemic lupus erythematosus.
Schur, P.H. & Hahn, B.H. (2021). Retrieved December 14, 2021
-UpToDateComplications of systemic lupus erythematosus in the emergency department.
Marco, J.L. & Chhakchhuak, C.L. (2018). Emergency Medicine. 50(1),6-16.
DOI: 10.12788/emed.2018.0075
Relevant Resources
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Jan 19, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.