Undifferentiated Shock – Diagnosis and Treatment
Cardinal Presentations / Presenting Problems, Critical Care / Resuscitation
Context
- Shock is a state of acute cardiocirculatory failure resulting in end-organ hypoxia and dysfunction.
- Promptly recognizing and treating shock is important as it is associated with high mortality
- Shock has many etiologies and is the final common pathway of death.
- Approach to undifferentiated shock requires simultaneous resuscitation and investigation.
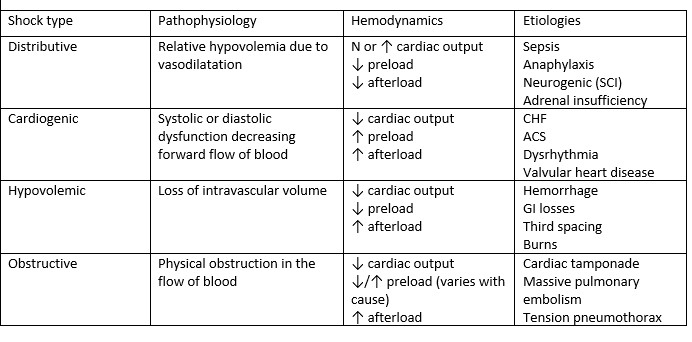
Table 1 Categories of shock
Diagnostic Process
Approach to undifferentiated shock
- Recognize shock.
- No single clinical finding or investigation can rule in or rule out shock. Diagnosis is based on a combination of clinical findings.
- Shock is commonly associated with hypotension, but it can also occur with normal blood pressure.
- Shock red flags
- Ill appearance.
- Altered mental status.
- HR > 100, MAP < 65, SBP < 90, shock index (SI) > 0.8.
- RR > 20.
- Urine output < 0.5 ml/kg/h.
- Skin – cool peripheries, mottling, urticaria.
- Lactate > 4 mM/L or arterial base deficit < -4mEq/L.
- Primary survey (ABCDE)
- Airway: assess airway patency.
- Breathing: assess oxygenation and ventilation.
- Consider the need for intubation and mechanical ventilation. Minimize induction agents to avoid hemodynamic collapse.
- Circulation: assess pulse, BP, telemetry, signs of obvious bleeding.
- Obtain large bore peripheral IV access. Obtain intraosseous access if peripheral IV access is difficult. Do not delay resuscitation for central line access.
- Disability: assess for level of consciousness and signs of spinal cord injury.
- Exposure: assess skin for urticaria, angioedema (signs of anaphylaxis).
- Rule out conditions requiring immediate intervention: tension pneumothorax, massive hemothorax, cardiac tamponade, MI, significant arrhythmias, massive PE, anaphylaxis, hypovolemia.
- Initiate empiric resuscitation unless the cause of shock is clear and is rapidly reversed.
- Fluid resuscitation.
- Fluid challenge with 300-500 ml of a crystalloid solution over 20-30 min. Repeat according to fluid responsiveness based on changes in BP, HR, urine output.
- Be cautious with excessive fluid administration, especially if suspecting cardiogenic shock or massive PE.
- Colloids like albumin are theoretically better intravascular volume expanders but there is no evidence of mortality benefit over crystalloids.
- Consider vasoactive agents if hypotension persists (MAP <65) despite fluid resuscitation.
- Typical first line agent is norepinephrine with initial dose of 0.2 mcg/kg/min. Norepinephrine can initially be given through peripheral IV until central line access is available.
- Vasopressin and epinephrine infusions can be used as second-line agents for severe cases of shock.
- Consider the use of inotropes if suspecting cardiogenic shock. Dobutamine is commonly used as a first line agent.
- Start broad-spectrum antibiotics if suspecting sepsis. Early antibiotic therapy improves outcomes in sepsis.
- Consider empiric corticosteroids for chronic steroid users or shock refractory to vasopressors and fluid resuscitation. Options include dexamethasone 6 mg IV or hydrocortisone 100 mg IV.
- Sodium bicarbonate therapy for severe metabolic acidosis is commonly used but there is no evidence of mortality benefit.
- Secondary survey focused on determining the cause of shock.
- History: trauma, infection, immunosuppression, corticosteroid use, exposure to allergen, chest pain, toxic ingestions.
- Head to toe examination.
- Point of care ultrasound (FAST, RUSH).
- Recent systematic review suggests ultrasound measurement of IVC is not a reliable indicator of volume status.
- Suggested initial investigations.
- Blood tests: ABG, lactate, CBC, serum chemistry, LFT, troponin, BNP, coagulation studies.
- ECG – ACS.
- CXR – heart failure or pneumonia.
- CT scan depending on working differential.
- Consider placing arterial line and/or central line.
- Reassess indicators of adequate hemodynamic support.
- MAP > 65 with clinical signs of adequate tissue perfusion (mental status, skin appearance, urine output).
- Decreasing serial lactate measurements.
6. Transition to ICU.
Quality Of Evidence?

High
We are highly confident that the true effect lies close to that of the estimate of the effect. There is a wide range of studies included in the analyses with no major limitations, there is little variation between studies, and the summary estimate has a narrow confidence interval.
Moderate
We consider that the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. There are only a few studies and some have limitations but not major flaws, there are some variations between studies, or the confidence interval of the summary estimate is wide.
Low
When the true effect may be substantially different from the estimate of the effect. The studies have major flaws, there is important variations between studies, of the confidence interval of the summary estimate is very wide.
Justification
Substantial evidence on the diagnosis and management of shock. Most clinical trials are specific to the ICU but of high quality.
Related Information
Reference List
Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013 Oct 31;369(18):1726-34. doi: 10.1056/NEJMra1208943. PMID: 24171518.
Annane D, Siami S, Jaber S, Martin C, Elatrous S, Declère AD, Preiser JC, Outin H, Troché G, Charpentier C, Trouillet JL, Kimmoun A, Forceville X, Darmon M, Lesur O, Reignier J, Abroug F, Berger P, Clec’h C, Cousson J, Thibault L, Chevret S; CRISTAL Investigators. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. JAMA. 2013 Nov 6;310(17):1809-17. doi: 10.1001/jama.2013.280502.
Jaber S, Paugam C, Futier E, Lefrant JY, Lasocki S, Lescot T, Pottecher J, Demoule A, Ferrandière M, Asehnoune K, Dellamonica J, Velly L, Abback PS, de Jong A, Brunot V, Belafia F, Roquilly A, Chanques G, Muller L, Constantin JM, Bertet H, Klouche K, Molinari N, Jung B; BICAR-ICU Study Group. Sodium bicarbonate therapy for patients with severe metabolic acidaemia in the intensive care unit (BICAR-ICU): a multicentre, open-label, randomised controlled, phase 3 trial. Lancet. 2018 Jul 7;392(10141):31-40. doi: 10.1016/S0140-6736(18)31080-8. Epub 2018 Jun 14. Erratum in: Lancet. 2018 Dec 8;392(10163):2440. PMID: 29910040.
Orso D, Paoli I, Piani T, Cilenti FL, Cristiani L, Guglielmo N. Accuracy of Ultrasonographic Measurements of Inferior Vena Cava to Determine Fluid Responsiveness: A Systematic Review and Meta-Analysis. J Intensive Care Med. 2020 Apr;35(4):354-363. doi: 10.1177/0885066617752308. Epub 2018 Jan 17. PMID: 29343170.
Evans, Laura1; Rhodes, Andrew2; Alhazzani, Waleed3; Antonelli, Massimo4; Coopersmith, Craig M.5; French, Craig6; Machado, Flávia R.7; Mcintyre, Lauralyn8; Ostermann, Marlies9; Prescott, Hallie C.10; Schorr, Christa11; Simpson, Steven12; Wiersinga, W. Joost13; Alshamsi, Fayez14; Angus, Derek C.15; Arabi, Yaseen16; Azevedo, Luciano17; Beale, Richard18; Beilman, Gregory19; Belley-Cote, Emilie20; Burry, Lisa21; Cecconi, Maurizio22; Centofanti, John23; Coz Yataco, Angel24; De Waele, Jan25; Dellinger, R. Phillip26; Doi, Kent27; Du, Bin28; Estenssoro, Elisa29; Ferrer, Ricard30; Gomersall, Charles31; Hodgson, Carol32; Hylander Møller, Morten33; Iwashyna, Theodore34; Jacob, Shevin35; Kleinpell, Ruth36; Klompas, Michael37; Koh, Younsuck38; Kumar, Anand39; Kwizera, Arthur40; Lobo, Suzana41; Masur, Henry42; McGloughlin, Steven43; Mehta, Sangeeta44; Mehta, Yatin45; Mer, Mervyn46; Nunnally, Mark47; Oczkowski, Simon48; Osborn, Tiffany49; Papathanassoglou, Elizabeth50; Perner, Anders51; Puskarich, Michael52; Roberts, Jason53; Schweickert, William54; Seckel, Maureen55; Sevransky, Jonathan56; Sprung, Charles L.57; Welte, Tobias58; Zimmerman, Janice59; Levy, Mitchell60 Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021, Critical Care Medicine: November 2021 – Volume 49 – Issue 11 – p e1063-e1143
doi: 10.1097/CCM.0000000000005337
Related Information
OTHER RELEVANT INFORMATION
RESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated Feb 17, 2022
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.