UA/NSTEMI – Management
Cardinal Presentations / Presenting Problems, Cardiovascular, Critical Care / Resuscitation
Context
Unstable Angina (UA) and NSTEMI frequently are difficult to distinguish at initial presentation, and therefore often considered together. The pathophysiology is the same, therefore initial management is also the same.
The same principles of early reperfusion and revascularization also apply.
- Goals of acute management include:
- Assessing and managing hemodynamic changes, treating ischemic pain, early risk stratification, choosing medical and/or invasive therapeutic interventions.
- 65% of myocardial infarctions occur in ages ≥ 65.
- > 75 years of age associated with more NSTEMI (compared to STEMI), atypical presentations, higher mortality, increased heart failure.
- Age is not an indication to withhold recommended NSTEMI therapy as this is correlated with higher in-hospital mortality.
- With cocaine-associated myocardial infarction, avoid beta-blockers as can exacerbate coronary artery vasoconstriction through unopposed activity.
Long-term therapeutic strategies – antiplatelet therapy, statins, oral anticoagulation, antihypertensive medications – are not covered in this summary.
Recommended Treatment
General Principles of Initial Management:
- Stabilize ABC’s, IV access.
- Optimal initial therapy initiated with the diagnostic approach.
- Anti-ischemic and Analgesic Therapy:
-
- Oxygen
- Use in patients with saturations < 92% or respiratory distress.
- Otherwise no benefit and theoretical worsening.
- Oxygen
-
- Nitroglycerin (NTG)
- Sublingual NTG 0.4 mg q 5 minutes up to three times unless relieves pain.
- IV NTG can be used if pain persists.
- Use with caution in:
- Inferior or RV ischemia, severe aortic stenosis.
- Use of phosphodiesterase inhibitors (e.g. sildenafil citrate, vardenafil hydroxide, tadalafil in the past 24 hours).
- Nitroglycerin (NTG)
-
- Morphine
- IV morphine is reserved for patients with severe pain.
- Use with caution (negative outcome effects seen in CRUSADE study).
- Can consider 2-4 mg IV slow push q5-15min
- Morphine
-
- Beta-Blockers
- If no contraindications, use in all patients within 24 hours of presentation.
- Cardioselective agents are preferred (e.g. metoprolol, atenolol).
- Metoprolol 25 mg PO BID (hold if systolic BP < 90 mmHg or HR < 50).
- Beta-Blockers
-
- Statin Therapy
- Treat with high-intensity statin therapy, regardless of baseline LDL levels.
- Options include Atorvastatin 80 mg daily, Rosuvastatin 40 mg daily.
- Statin Therapy
-
- Antithrombotic Therapy in all patients (without absolute contraindications):
- Dual Antiplatelet Therapy (DAPT):
- *Aspirin 162 – 325 mg, chew and swallow (unless considering aortic dissection).
- Consider early administration of this medication even prior to a definitive diagnosis.
- *Aspirin 162 – 325 mg, chew and swallow (unless considering aortic dissection).
- Dual Antiplatelet Therapy (DAPT):
- Antithrombotic Therapy in all patients (without absolute contraindications):
- P2Y12 inhibitor (eg. Clopidogrel, Ticagrelor, Prasugrel).
*ONLY if not likely to go to CABG in next 5 days**NEW** in Vancouver Coastal April 2021.- Consider Ticagrelor – start with a loading dose of 180 mg, then 90 mg BID.
- Can be used in patients managed with or without invasive revascularization.
- Can consider Clopidogrel 300 mg PO, then 75 mg PO daily.
- Clarify with local interventionalist.
- Anticoagulation:
- If the patient is for an early invasive procedure within 48 h consider unfractionated heparin.
- Use Heparin ACS Nomogram to determine Heparin IV bolus followed by IV infusion.
- If the patient is for an early invasive procedure within 48 h consider unfractionated heparin.
- If the patient being managed only medically, consider LMWH with Enoxaparin or Fondaparinux.
- Enoxaparin 1 mg/kg, max 120 mg SC q12h (if eGFR < 30 mL/min then q24h).
- ACE Inhibitors2:
- Unless contraindicated, use in patients with EF < 40%, HTN, diabetes, CKD.
Note: NSAIDs (other than ASA) should be discontinued.
Note: Experts recommend ensuring adequate serum levels of Potassium and Magnesium.
Note: Treat left heart failure if present: afterload reduction with Nitroglycerin (if no hypotension or phosphodiesterase inhibitors), IV Furosemide, BiPAP.
Note: NSTEMI’s can result in atrial and ventricular arrhythmias. These include atrial fibrillation or flutter, and ventricular tachycardia or ventricular fibrillation. “Recommended prophylactic measures include early administration of a beta blocker and treatment of hypokalemia and hypomagnesemia.
Note: For cocaine associated ACS provide benzodiazepines (eg. Lorazepam 2-4 mg IV q 15 mins PRN).
Principles of Early Reperfusion and Revascularization in NSTEMI/UA3
- Fibrinolysis avoided in UA/NSTEMI: no benefit.
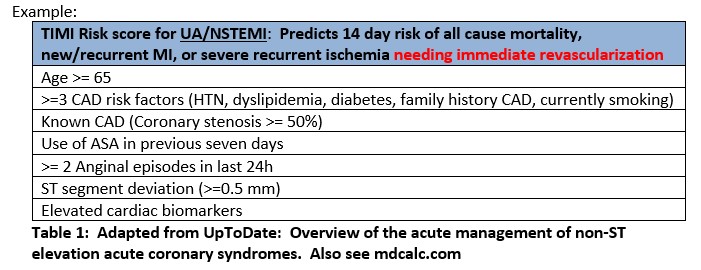
- Risk stratification after diagnosis helps determine if revascularization should be performed and, if yes, the timing of revascularization. Use tools like TIMI and GRACE (*caution; use judgment as these are not perfect).
- Categorize into immediate angiography, invasive approach (early invasive approach, delayed invasive approach), conservative.
- Immediate angiography and revascularization when cardiogenic shock, heart failure, persistent angina, sustained ventricular arrhythmias, dynamic ST-T wave ECG changes.
- Invasive Approach aimed at improving long-term prognosis. Revascularization is intended within 4-48h of admission.
- Revascularization intended within 24h (early) vs within 48h (delayed).
- Conservative strategy – These patients are deemed to be low risk and receive rapid medical therapy. Patients who are asymptomatic can then have left ventricular function, and stress testing (often with a form of myocardial imaging) within a near date (note: for patients for whom revascularization is reasonable, stress testing is performed before or within 48h of discharge). However, the persistence of symptoms, recurrence of symptoms, or development of high-risk predictors should lead to prompt revascularization.
*Note: Severe co-morbidities may prevent suitability for revascularization.
Criteria For Hospital Admission
- All UA/NSTEMI patients should be admitted for further work-up and cardiac stabilization. Recommend Cardiology Consultation.
- 1Risk Stratification can potentially identify patients at risk for further cardiac events. It can be a tool to determine who may benefit from urgent revascularization.
- Risk factors include the presence and amount of ST-segment depression, troponin elevation, hemodynamic instability, persistent chest pain despite medical therapy.
- Risk scores include TIMI, GRACE, PURSUIT (see mdcalc.com5).
*This summary refers to the acute management of UA/NSTEMI. Long-term management of UA/NSTEMI is not covered.
Related Information
Reference List
Overview of the acute management of non-ST elevation acute coronary syndromes.
Hooton TM, Gupta K. Post, TW (Ed), UpToDate, Waltham, MA, 2020
-UpToDateNon ST Segment Elevation Myocardial Infarction.
Basit H, Malik A, Huecker MR. [Updated 2020 Oct 15]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-.
– StatPearls [Internet]Acute ST-elevation myocardial infarction: Selecting a reperfusion strategy.
Hooton TM, Gupta K. Post, TW (Ed), UpToDate, Waltham, MA, 2020.
-UpToDate-
Relevant Resources
RELEVANT RESEARCH IN BC
Cardiovascular EmergenciesRESOURCE AUTHOR(S)

DISCLAIMER
The purpose of this document is to provide health care professionals with key facts and recommendations for the diagnosis and treatment of patients in the emergency department. This summary was produced by Emergency Care BC (formerly the BC Emergency Medicine Network) and uses the best available knowledge at the time of publication. However, healthcare professionals should continue to use their own judgment and take into consideration context, resources and other relevant factors. Emergency Care BC is not liable for any damages, claims, liabilities, costs or obligations arising from the use of this document including loss or damages arising from any claims made by a third party. Emergency Care BC also assumes no responsibility or liability for changes made to this document without its consent.
Last Updated May 16, 2021
Visit our website at https://emergencycarebc.ca
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.