Interior Health is making an impact on patients with AUD through brief targeted interventions in the ED
Many of us enjoy sitting down for a delicious craft beer or fine glass of wine. However, as emergency department (ED) practitioners, we are also acutely aware of the life-altering consequences alcohol can have. People with Alcohol Use Disorder (AUD) are 4.4 times more likely to visit an ED than the general population. Additionally, 25% of all ED visits involve patients who screen positive for problematic alcohol use, with a striking 70% of those visits occurring among individuals aged 12-24.
Although our core work in the ED is managing and stabilizing critically ill patients, we also have an opportunity to impact patient health through brief targeted interventions. Naltrexone and Acamprosate are relatively new and effective treatments for patients with AUD who are working to achieve abstinence with a Number Needed to Treat (NNT) of 20 and 12 respectively. A brief intervention conversation with a patient struggling with AUD may be a life changing moment for them.
Showcasing the Work
AUD in ED is a project that originated as a partnership between the IH Emergency Services Network and the Mental Health and Substance Use (MHSU) Transformation Team, following initial pilot efforts by the late Dr. Jeff Harries. The objective of the pilot was to identify patients with AUD and provide prescriptions for Naltrexone and Acamprosate. Our expanded IH-led AUD in ED initiative has expanded goals including systematic screening for AUD, timely interventions, and seamless integration of treatment pathways to support both patients and emergency providers, addressing the full continuum of alcohol-related presentations to our EDs.
Tools, Approaches, and Learnings for Broader Implementation
1. Comprehensive Toolkit
A toolkit is an essential part of the AUD program aimed at improving care for patients who present to the ED. Included in the toolkit:
a. AUD in ED Workflow: A clear, structured process for ED staff to follow when assessing and managing patients with high-risk drinking/AUD. This workflow ensures that each step in the diagnosis, treatment, and follow-up care is standardized, leading to more efficient and effective care.
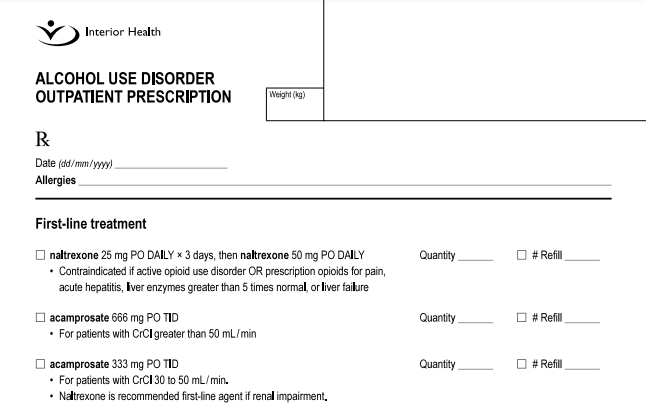
b. AUD Pharmacotherapy Guidelines and Prescription Template: These guidelines provide evidence-based recommendations for prescribing medications to treat AUD. The prescription template helps clinicians issue appropriate medication prescriptions, which streamlines the process and promotes consistency in treatment.
c. Conversation Guide: This guide offers ED staff communication strategies to engage with patients about their substance use. It includes tips on how to approach sensitive conversations in a non-judgmental and supportive manner, addressing stigma while building rapport and trust.
d. Withdrawal Management Order Sets: These order sets provide clear, pre-determined instructions for managing alcohol withdrawal symptoms, ensuring that staff can quickly and appropriately intervene to manage withdrawal in patients.
e. Patient Information Sheets: These sheets give patients information about available resources for ongoing care and details about medications they may be prescribed. These tools were created in collaboration with People with Lived/Living Experience of alcohol use and treatment. These resources support patients to understand their treatment options and supports their engagement in care beyond the ED visit.
By providing these resources, the toolkit ensures that ED staff can consistently deliver high-quality, evidence-based care to patients with AUD, improving patient outcomes and ensuring safe, effective management of this condition.
2. Collaborative Care Pathways
The success of the program lies in its integrated care approach, which includes follow-up within 72 hrs through IH Virtual Addiction Medicine (VAM) clinic and/or local addiction medicine teams, community treatment programs, and inpatient acute treatment pathways. Ensuring patients have clear follow-up and support structures after ED visits reduces relapse risk and enhances long-term outcomes.
3. Training Modules and Support Resources
AUD in ED incorporates robust training, emphasizing patient-first language and culturally competent care, with educational materials available through IH platforms. eLearning modules cover essential practices like applying trauma-informed practice and providing culturally safe care. Program rollout is done in a phased approach, rather than “big-bang”, with introductory virtual meetings and then in-person delivery, with nurse to nurse & physician to physician engagement.
4. Learning from Barriers
IH experiences reveal that ongoing education and awareness campaigns are essential to tackle barriers such as stigma and limited provider engagement. Addressing these challenges with targeted outreach and feedback loops can lead to better staff participation and patient outcomes.
Impact and Evaluation
- Immediate Benefits: AUD in ED has already shown significant positive outcomes. Population data indicates that only 2% of eligible patients typically receive evidence-based pharmacotherapy for AUD, highlighting the dire need for targeted intervention. By implementing the program, IH data shows promising trends in patient engagement and treatment adherence. Notably, 56% of patients referred to VAM filled a prescription for relapse prevention within 90 days, with 32% doing so within the first week. This early intervention is crucial, as prompt access to pharmacotherapy significantly impacts outcomes. Additionally, 63% of surveyed patients rated their experience as “very good” or “good,” and 95% felt treated with courtesy and respect. These results reflect the project’s positive influence on patient trust and retention in treatment.
- Long-Term Prospects: AUD in ED’s impacts extend beyond immediate care to systemic improvements. Increased training and awareness among healthcare providers have begun to change how AUD is addressed. While challenges such as stigma and provider training remain, the project is setting groundwork for an enduring shift in patient treatment norms. Integration of trauma-informed practices and culturally safe environments is expected to further strengthen trust and care quality over time.
What Can I Do? Your Call to Action
Other health authorities across BC can leverage the IH strategies and insights to implement similar programs, ensuring that those struggling with AUD received timely, effective care and support.

RESOURCES:
REFERENCES:
- Pearson C, Janz T, Ali J. Mental and substance use disorders in Canada. Ottawa: Health at a Glance — Statistics Canada; 2015. Cat. no. 82-624-X. Available: https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11855-eng.htm (accessed 2023 May 10).Google Scholar
- Paradis C, Butt P, Shield K, et al. Canada’s guidance on alcohol and health: final report. Ottawa: Canadian Centre on Substance Use and Addiction; 2023. Available: https://ccsa.ca/sites/default/files/2023-01/CCSA_Canadas_Guidance_on_Alcohol_and_Health_Final_Report_en.pdf (accessed 2023 May 10).
- Shield K, Manthey J, Rylett M, et al. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: a comparative risk assessment study. Lancet Public Health 2020;5:e51–61.
- Rehm J, Mathers C, Popova S, et al. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009;373:2223–33.CrossRefPubMedGoogle Scholar
- Konrad G, Leong C, Bolton JM, et al. Use of pharmacotherapy for alcohol use disorder in Manitoba, Canada: a whole-population cohort study. PLoS One 2021;16:e0257025.Google Scholar
- Spithoff S, Turner S, Gomes T, et al. First-line medications for alcohol use disorders among public drug plan beneficiaries in Ontario. Can Fam Physician 2017;63:e277–83.Abstract/FREE Full TextGoogle Scholar
- Kranzler HR, Soyka M. Diagnosis and pharmacotherapy of alcohol use disorder: a review. JAMA 2018;320:815–24.CrossRefGoogle Scholar
- Chick J. Unhelpful prescribing in alcohol use disorder: risk and averting risk. Alcohol Alcohol 2019;54:1–4.Google Scholar https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/sfv-avf/sources/fem/fem-intin-alco/pdf/fem-whoms-alco-eng.pdf
- Myran, Daniel T, et al. Rates of emergency department visits attributable to alcohol use in Ontario from 2003 to 2016: A retrospective population – level study. Canadian Medical Association Journal. 2019.
- British Columbia Centre on Substance Use (BCCSU), B.C. Ministry of Health and B.C. Ministry of Mental Health and Addictions. Provincial Guideline for the Clinical Management of High-Risk Drinking and Alcohol Use Disorder. [Online] 2019. https://www.bccsu.ca/alcohol-use-disorder/.
- Kranzler, Henry R and Soyka, Michael. Diagnosis and Pharmacotherapy of Alcohol Use Disorder: A Review. JAMA. 2018, Vol. 320, 8, pp. 815-824.
- BC Coroners Service . Illicit Drug Toxicity Deaths in BC January 1, 2021 – August 31, 2022. 2022.
- Canadian Evaluation Society. (n.d.). Evaluation Standards. Retrieved March 1, 2023, from https://evaluationcanada.ca/career/evaluation-standards.html
COMMENTS (0)
Add public comment…



POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.