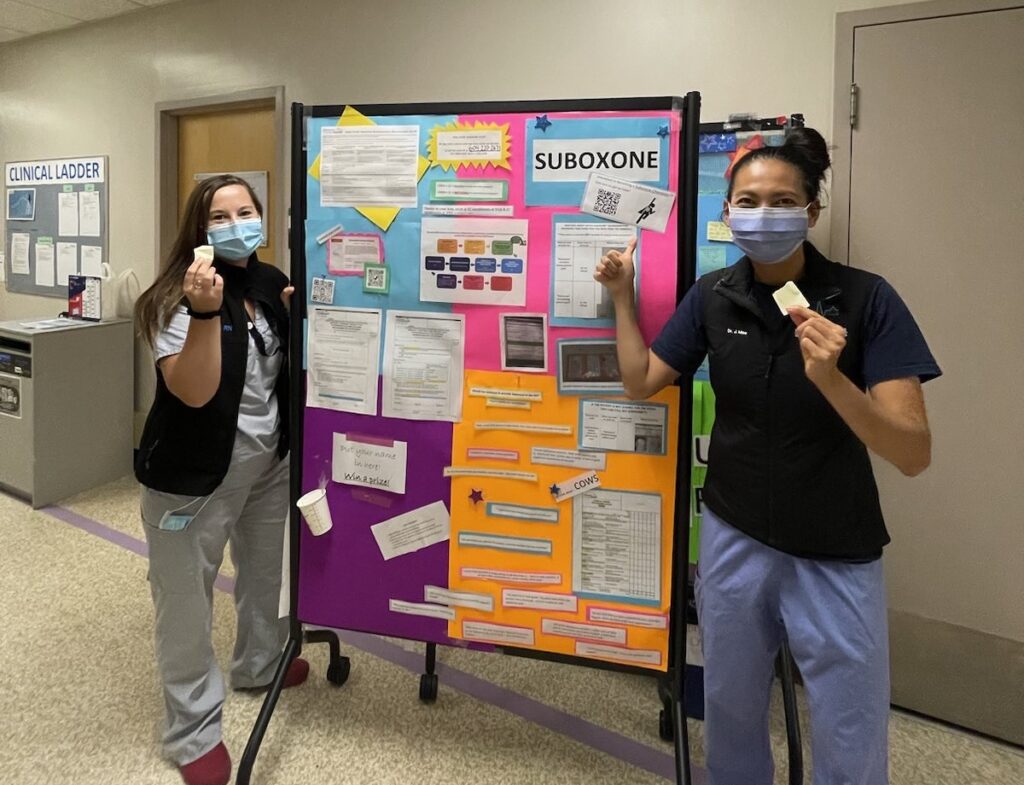
Primary Author: Gilbert Lee | Supervising Author: Dr. Jessica Moe
In Canada, opioid-related deaths claimed over 36,000 lives between January 2016 and December 2022, with the number of deaths per year having doubled within this time frame.1,2 Further, emergency department (ED) visits are common in patients who later overdose, creating critical intervention opportunities.3
Buprenorphine, a first-line opioid agonist therapy (OAT), can reduce illicit opioid use and is safe in take-home regimens but requires patients to be in withdrawal before induction to prevent precipitated withdrawal.4-6 Novel microdosing approaches allow continued opioid use while titrating the medication, mitigating this uncomfortable barrier to initiation.7,8
The EMED (Evaluating Microdosing in the Emergency Department) Study is being conducted by a study team led by Dr. Jessica Moe at UBC and compares the effectiveness of ED-initiated buprenorphine/naloxone (Suboxone) microdosing and standard dosing take-home inductions. The study will measure completions of the induction period and retention on OAT (via provincial pharmacy records), reductions in overdose & mortality, and healthcare utilization.
Patients 18 years or older with opioid-use disorder (using the validated Rapid Opioid Dependence Screen) and not receiving OAT are eligible for the study. Candidates are screened and randomly placed into two treatment groups:
- Standard Induction: Patients must abstain from opioid use for at least 24 hours and experience moderate/severe withdrawal before initiation.
- Day 1: buprenorphine 2 mg (1 tablet) per hour until symptoms improve (to a maximum of 6 tablets).
- Day 2: buprenorphine 12 mg (6 tablets) once daily.
- Days 3-5: buprenorphine 16 mg (8 tablets) once daily.
- Microdosing Induction: Patients do not need to be in withdrawal before induction and must continue using opioids while titrating the initial doses of Suboxone to prevent withdrawal.
- Day 1: buprenorphine 0.5 mg (¼ tablet) four times daily.
- Day 2: buprenorphine 1 mg (½ tablet) four times daily.
- Day 3: buprenorphine 2 mg (1 tablet) four times daily.
- Day 4: buprenorphine 3 mg (1½ tablets) four times daily.
- Day 5: buprenorphine 16 mg (8 tablets) once daily.
* Although microdosing regimens have not been approved of broadly for clinical practice, Health Canada has approved of this protocol for the purposes of the EMED Study.
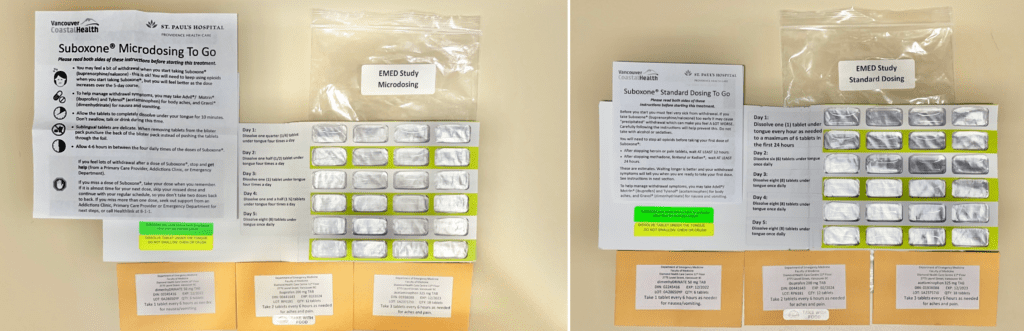
Healthcare providers counsel all patients on Suboxone usage prior to discharging them with a five-day supply of Suboxone, adjunctive medications (e.g., ibuprofen, acetaminophen, dimenhydrinate) to relieve withdrawal symptoms, Naloxone & sterile injection kits if desired, and follow-up clinic information to discuss continued treatment with an addictions specialist.
During the study, the team collects baseline data on demographics, health, socioeconomic status, substance use, and treatment history. The team conducts five days of phone/text follow-up to collecting information about the patient’s experience with Suboxone, continued treatment plans, and their ED/enrollment experience.
Collaborating with Vancouver Coastal Health’s Overdose Outreach Team, the team conducts follow-ups within 30 days of enrollment, to assess patients’ needs and monitor any serious adverse events.
As of July 2023, we have three sites in BC and one site in Alberta. The team has screened 10,715 and enrolled 192 patients across four sites, with 91 receiving standard dosing and 101 receiving microdosing. The team has reached 60 enrolled patients for follow-up and the Overdose Outreach Team has reached 26.
*Screened patients are those who have had their study eligibility assessed by the study team. These include patients who come to the emergency room with a chief complaint of localized swelling and redness, overdose, withdrawal, cellulitis, or intoxication/substance misuse, or those who have been identified as a potential study candidate by a healthcare provider.
*Enrolled patients are those who have met our study eligibility requirements, consented to participate, were randomized into one of the treatment arms, and received their medication.
If you are interested in being a participating site, please contact emed.study@ubc.ca or Dr. Jessica Moe at jessica.moe@ubc.ca.
References
- Opioid- and stimulant-related harms [Internet]. Government of Canada; 2023 [cited 2023 Jul 16]. Available from: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants
- Canada H. Modelling opioid-related deaths during the overdose crisis [Internet]. Government of Canada; 2023 [cited 2023 Jul 16]. Available from: https://www.canada.ca/en/health-canada/services/opioids/data-surveillance-research/modelling.html
- Otterstatter MC, Crabtree A, Dobrer S, Kinniburgh B, Klar S, Leamon A, et al. Patterns of health care utilization among people who overdosed from illegal drugs: A descriptive analysis using the BC provincial overdose cohort. Health Promotion and Chronic Disease Prevention in Canada. 2018;38(9):328–38. doi:10.24095/hpcdp.38.9.04
- D’Onofrio G, O’Connor PG, Pantalon MV, Chawarski MC, Busch SH, Owens PH, et al. Emergency department–initiated buprenorphine/naloxone treatment for opioid dependence. JAMA. 2015;313(16):1636. doi:10.1001/jama.2015.3474
- Walsh SL, Preston KL, Stitzer ML, Cone EJ, Bigelow GE. Clinical pharmacology of buprenorphine: Ceiling effects at high doses. Clinical Pharmacology and Therapeutics. 1994;55(5):569–80. doi:10.1038/clpt.1994.71
- The Asam National Practice Guideline for the treatment of opioid use disorder: 2020 focused update. Journal of Addiction Medicine. 2020;14(2S):1–91. doi:10.1097/adm.0000000000000633
- Adams KK, Machnicz M, Sobieraj DM. Initiating buprenorphine to treat opioid use disorder without prerequisite withdrawal: A systematic review. Addiction Science & Clinical Practice. 2021;16(1). doi:10.1186/s13722-021-00244-8
- Hämmig R, Kemter A, Strasser J, von Bardeleben U, Gugger B, Walter M, et al. Use of microdoses for induction of buprenorphine treatment with overlapping full opioid agonist use: The Bernese method. Substance abuse and rehabilitation 2016;7:99-105. doi:10.2147/sar.s109919
COMMENTS (0)
Add public comment…


POST COMMENT
We welcome your contribution! If you are a member, log in here. If not, you can still submit a comment but we just need some information.